Articles
- Page Path
- HOME > Acute Crit Care > Volume 35(3); 2020 > Article
-
Original Article
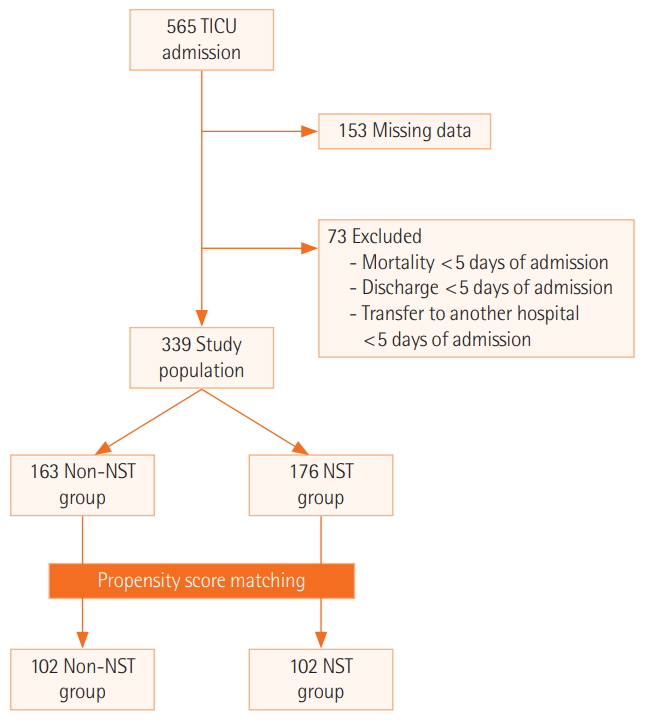
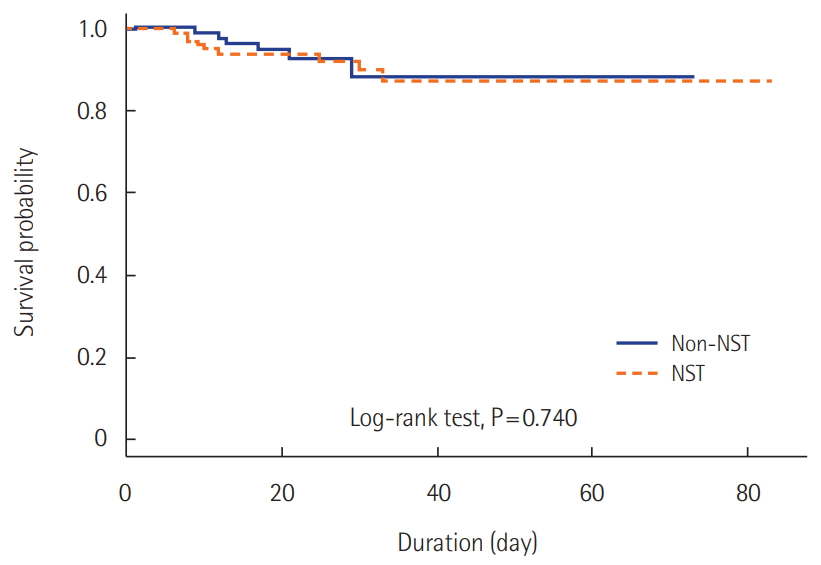
Nutrition Effectiveness of a multidisciplinary team for nutrition support in a trauma intensive care unit -
Eunsuk Oh1,2
 , Hongjin Shim1,3,4
, Hongjin Shim1,3,4 , Hyon Ju Yon1,5
, Hyon Ju Yon1,5 , Jin Sil Moon6
, Jin Sil Moon6 , Dae Ryong Kang6
, Dae Ryong Kang6 , Ji Young Jang7
, Ji Young Jang7
-
Acute and Critical Care 2020;35(3):142-148.
DOI: https://doi.org/10.4266/acc.2020.00318
Published online: August 19, 2020
1Nutrition Support Team, Wonju Severance Christian Hospital, Wonju, Korea
2Dapartment of Pharmacy, Wonju Severance Christian Hospital, Wonju, Korea
3Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
4Trauma Center, Wonju Severance Christian Hospital, Wonju, Korea
5Department of Nutrition Services, Wonju Severance Christian Hospital, Wonju, Korea
6Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
7Department of Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- Corresponding author Ji Young Jang Department of Surgery, National Health Insurance Service Ilsan Hospital, 100 Ilsan-ro, Ilsandong-gu, Goyang 10444, Korea Tel: +82-31-900-0975 Fax: +82-31-900-0138 E-mail: drjangjiyoung@gmail.com
Copyright © 2020 The Korean Society of Critical Care Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Impact of a multidisciplinary collaborative nutritional treatment model in patients who are critically ill with neurological disorders: A randomized controlled trial
Bao-Di Gu, Yun Wang, Rong Ding
Technology and Health Care.2024; 32(3): 1767. CrossRef - Implementation of a multidisciplinary nutritional support team and clinical outcomes in critically ill patients with COVID-19
In-Ae Song, Kyunghwa Lee, Sunghee Lee, Keonhee Kim, Tak Kyu Oh
Clinical Nutrition.2024; 43(2): 315. CrossRef - Nutrition support teams: Institution, evolution, and innovation
Albert Barrocas, Denise Baird Schwartz, Bruce R. Bistrian, Peggi Guenter, Charles Mueller, Ronni Chernoff, Jeanette M. Hasse
Nutrition in Clinical Practice.2023; 38(1): 10. CrossRef - Multidisciplinary Difficult Airway Team Characteristics, Airway Securement Success, and Clinical Outcomes: A Systematic Review
Vinciya Pandian, Talha U. Ghazi, Marielle Qiaoshu He, Ergest Isak, Abdulmalik Saleem, Lindsay R. Semler, Emily C. Capellari, Michael J. Brenner
Annals of Otology, Rhinology & Laryngology.2023; 132(8): 938. CrossRef - Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients
Seunghyun Cheon, Sang-Hyeon Oh, Jung-Tae Kim, Han-Gon Choi, Hyojung Park, Jee-Eun Chung
Nutrients.2023; 15(11): 2531. CrossRef - Consultation pattern changes of parenteral nutrition with a multidisciplinary nutrition support team in a recently opened hospital in Korea: a retrospective cohort study
Kyoung Won Yoon, Hyo Jin Kim, Yujeong Im, Seul Gi Nam, Joo Yeon Lee, Hyo Gee Lee, Joong-Min Park
Annals of Clinical Nutrition and Metabolism.2023; 15(2): 57. CrossRef - Lipid emulsion treatment of cardiotoxicity caused by calcium channel blocker and beta-blocker
Ju-Tae Sohn
The American Journal of Emergency Medicine.2022; 58: 331. CrossRef - Physician Compliance with Nutrition Support Team Recommendations: Effects on the Outcome of Treatment for Critically Ill Patients
Hyon-Ju Yon, Eun-Suk Oh, Ji Young Jang, Ji Yun Jang, Hongjin Shim
Journal of Acute Care Surgery.2022; 12(1): 1. CrossRef - Nutritional Status of Intensive Care Unit Patients According to the Referral to the Nutrition Support Team and Compliance with the Recommendations
Yunjin Sohn, Taisun Hyun
Korean Journal of Community Nutrition.2022; 27(2): 121. CrossRef - Lipid emulsion dosage used for resuscitation after drug toxicity
Ju-Tae Sohn
The American Journal of Emergency Medicine.2022; 59: 168. CrossRef - Intensive care management of traumatic brain injury: How can mnemonics help?
Biljana Damnjanović, Jovana Stanisavljević, Adi Hadžibegović, Ivan Rović, Đuro Šijan, Nemanja Jovanović, Sanja Ratković, Marija Milenković
Serbian Journal of Anesthesia and Intensive Therapy.2022; 44(5-6): 105. CrossRef - 救急・集中治療領域 重症患者における栄養管理
信人 中西, 穣治 小谷
The Japanese Journal of SURGICAL METABOLISM and NUTRITION.2022; 56(6): 229. CrossRef - Urinary Titin N-Fragment as a Biomarker of Muscle Atrophy, Intensive Care Unit-Acquired Weakness, and Possible Application for Post-Intensive Care Syndrome
Nobuto Nakanishi, Rie Tsutsumi, Kanako Hara, Masafumi Matsuo, Hiroshi Sakaue, Jun Oto
Journal of Clinical Medicine.2021; 10(4): 614. CrossRef - Lack of evidence for a nutritional support team in a trauma intensive care unit?
Jae Hwa Cho
Acute and Critical Care.2020; 35(3): 205. CrossRef
- Figure
- Related articles
-
- Corrigendum to: Development of a deep learning model for predicting critical events in a pediatric intensive care unit
- Development of a deep learning model for predicting critical events in a pediatric intensive care unit
- Radiomic analysis of abdominal organs during sepsis of digestive origin in a French intensive care unit
- Digital tomography in the diagnosis of a posterior pneumothorax in the intensive care unit

 KSCCM
KSCCM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite