Abstract
-
Background
- The use of intravenous immunoglobulin (IVIG) in sepsis patients from bowel perforation is still debatable. However, few studies have evaluated the effect of IVIG as an adjuvant therapy after source control. This study aimed to analyze the effect of IVIG in critically ill patients who underwent surgery due to secondary peritonitis.
-
Methods
- In total, 646 medical records of surgical patients who were treated for secondary peritonitis were retrospectively analyzed. IVIG use, initial clinical data, and changes in Sequential Organ Failure Assessment (SOFA) score over the 7-day admission in the intensive care unit for sepsis check, base excess, and delta neutrophil index (DNI) were analyzed. Mortalities and periodic profiles were assessed. Propensity scoring matching as comparative analysis was performed in the IVIG group and non-IVIG group.
-
Results
- General characteristics were not different between the two groups. The survival curve did not show a significantly reduced mortality in the IVIG. Moreover, the IVIG group did not have a lower risk ratio for mortality than the non-IVIG group. However, when the DNI were compared during the first 7 days, the reduction rate in the IVIG group was statistically faster than in the non-IVIG group (P<0.01).
-
Conclusions
- The use of IVIG was significantly associated with faster decrease in DNI which means faster reduction of inflammation. Since the immune system is rapidly activated, the additional use of IVIG after source control surgery in abdominal sepsis patients, especially those with immunocompromised patients can be considered. However, furthermore clinical studies are needed.
-
Keywords: intravenous immunoglobulin; mortality; neutrophil; peritonitis; sepsis
INTRODUCTION
Patients with secondary peritonitis show various clinical features from local inflammation to septic shock even though they underwent source control including surgery and appropriate antibiotics [1]. In particular, sepsis from peritonitis may be induced or relieved depending on the patient's immune system [2]. Recent studies have reported that increased immunoglobulin levels lead to a higher survival rate in patients with sepsis, raising interest in the inflammatory response and immune resistance [3,4]. Moreover, it has been reported that immunity can be increased by injecting immunoglobulin, and the effects of antibiotics can be amplified to treat sepsis [5]. Intravenous immunoglobulin (IVIG) administration during infection not only stimulates the patient’s immune function but also provides a synergistic effect that increases antibiotic effectiveness [6,7]. Studies have shown that IVIG lowered mortality in septic shock patients [8]. However, some studies had different results [9], thus, there are no clear conclusions about its effectiveness. A 2013 Cochrane review reported that polyclonal IVIG did not lower mortality rates in septic patients [8] and IVIG is not included in the treatment guidelines for patients with sepsis. Because most positive results were obtained from small-scale studies, evidence from large-scale studies recommending IVIG as a treatment is lacking [10].
Therefore, this study aimed to investigate the effects of IVIG use on the prognosis of patients who developed sepsis postoperatively secondary to peritonitis, taking into consideration hospital mortality, in-hospital 30-day mortality, survival curve, hospitalization duration, intensive care unit (ICU) stay, ventilation period, Sequential Organ Failure Assessment (SOFA) score, base excess (BE), and delta neutrophil index (DNI). The primary endpoint was to check the superior effect of IVIG for mortality and the secondary endpoint was to see the additional advantages of IVIG than control group.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Yonsei University Wonju College of Medicine (No. CR318137). The informed consent was waived due to the retrospective nature of the study.
Patient Selection and Criteria
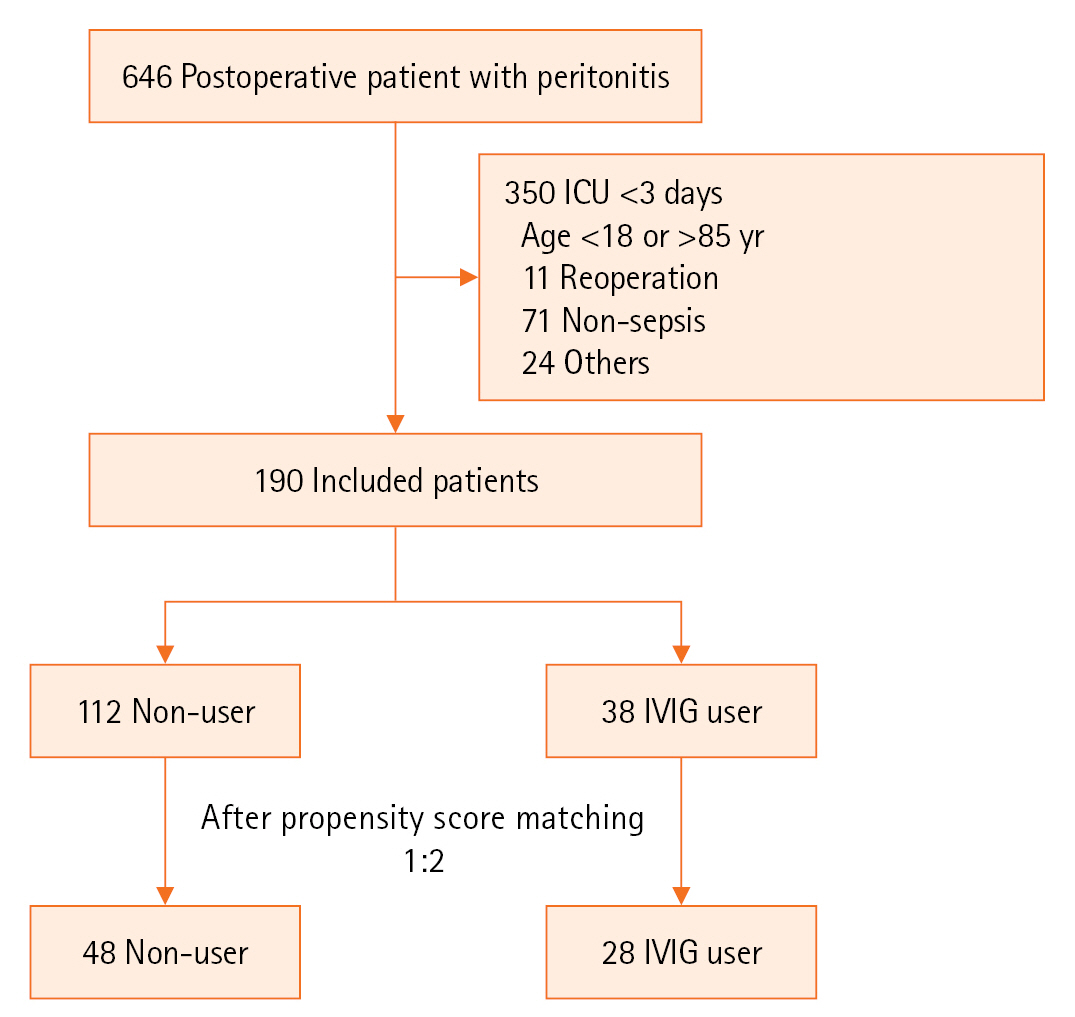
This study retrospectively identified 646 patients who received surgical treatment after diagnosis with secondary peritonitis from March 2013 to June 2018 and were treated in the ICU of a tertiary university hospital. To evaluate the effectiveness of IVIG, patients discharged from the ICU within 3 days and reoperation or non-sepsis cases were excluded. The specific inclusion criteria were as follows: adult patients aged 18–85 years who meet Sepsis-3 criteria, diagnosed with secondary peritonitis and treated in the ICU after surgical abdominal surgery. Specific exclusion criteria are shown in Table 1. Finally, 76 of 646 patients were included. Applying 1:2 propensity score matching and adjusting by age, sex, SOFA, APACHE II score, and time to operation after hospitalization, the number of IVIG group and non-IVIG group was 28 and 48, respectively.
IVIG Indications in Korea
In Korea, IVIG can be used in immunocompromised patients, such as those with sepsis, neonatal sepsis, and acquired immunodeficiency syndrome, and with potential complications when conventional treatments are ineffective, and it is covered by insurance. In severe sepsis, it can be used when the patient presents with more than two findings of systemic inflammatory response syndrome and more than one finding of multiple organ dysfunction syndrome (MODS). Signs of MODS include acute oliguria (urine output <0.5 ml/kg/hr for at least 2 hours), acute hypoxemia (PaO2/FiO2 <300), thrombocytopenia (platelet <100,000/µl), and lactic acidosis (lactate >2 mmol/L). IVIG administration during infection not only stimulates the patient’s immune function but also provides a synergistic effect that increases antibiotic effectiveness [6,7]. Thus, IVIG is recommended for use in combination with antibiotics, with a dose of 1 g/kg given over 3 days in Korea. In this study, patients who satisfied the IVIG indications were given the total dose within 3 days. They were defined as the IVIG group. Patients were defined as the non-IVIG group when, even though they met the requirements, their physician did not prefer it.
Effectiveness Evaluation Items
To evaluate the two groups, a comparative analysis was primarily carried out on the overall mortality rate, in-hospital mortality, hospitalization duration, 30-day mortality, survival curve, ICU stay, and ventilation period. Overall mortality was measure for patients confirmed on hospital charts by the time the study was conducted In addition, as an outcome variable for treatment, changes in the SOFA score, and DNI value on days 1, 3, and 7 since ICU admission were monitored. For the severity of the patient's condition, the initial APACHE II score within 24 hours from the emergency room to the ICU was used, along with the SOFA score on the first day of the ICU stay. To ensure that there were no errors in the use of antibiotics and source control (operation), which are recognized risk factors for death from sepsis, only patients who underwent emergency surgery by visiting the emergency room were targeted for inclusion. In addition, antibiotic start time and adequacy were investigated to ensure no difference between the two groups.
Delta Neutrophil Index
Delta neutrophil (DN) is a very sensitive indicator of the inflammatory response which uses immature granulocyte blood tests. For the identification of leukocytes, both basophil cytogram, an analysis method based on the size and shape of cells and nuclei, and peroxidase cytogram, a method using myeloperoxidase (MPO) reaction, were used. Polymorphonuclear cells are measured in the basophil cytogram, and DNs are measured as if they are components of the monocytes and are not present in the multinuclear cell region. Therefore, if the difference between the multinuclear cells measured by each method is calculated, the actual number of DN can be indirectly calculated. The calculation formula of DNI is as follows:
DNI=(leukocyte subfraction assayed in the MPO channel by cytochemical reaction)–(leukocyte subfraction counted in the nuclear lobularity channel by the reflected light beam).
Statistical Analysis
For continuous variables, data are expressed as the mean±standard deviation and median (range) using an unpaired t-test. For categorical variables, data are expressed as frequency and percentage and analyzed by the chi-square (or Fisher’s exact test). A propensity score for the predicted probability of IVIG users was estimated using the nearest-neighbor method through multivariable logistic regression model fit. The C-statistic of the logistic regression model for propensity score matching was 0.828, and the Hosmer-Lemeshow test P-value was 0.735. The adjusted covariates in the propensity score matching included age, sex, APACHE II score, SOFA score, and time to operation after hospitalization (Figure 1). The performance of the propensity score matching was evaluated by standard difference, and the absolute standard difference was confirmed to be within 10%. The stratified log-rank test was used to identify survival curves between IVIG and non-IVIG groups in the paired data, and the crude and adjusted hazard ratios (95% confidence interval [CI]) were estimated using the Cox proportional hazards model for the primary outcome. Adjusted variables are age, sex, APACHE Ⅱ score, and SOFA score. In addition, SOFA score and DNI were evaluated over time in the IVIG group using a linear mixed model. Analyses were performed using SAS 9.4 (SAS Institute) or SPSS for ver. 23.0 (IBM Corp.). A P<0.05 was established as the level of statistical significance.
RESULTS
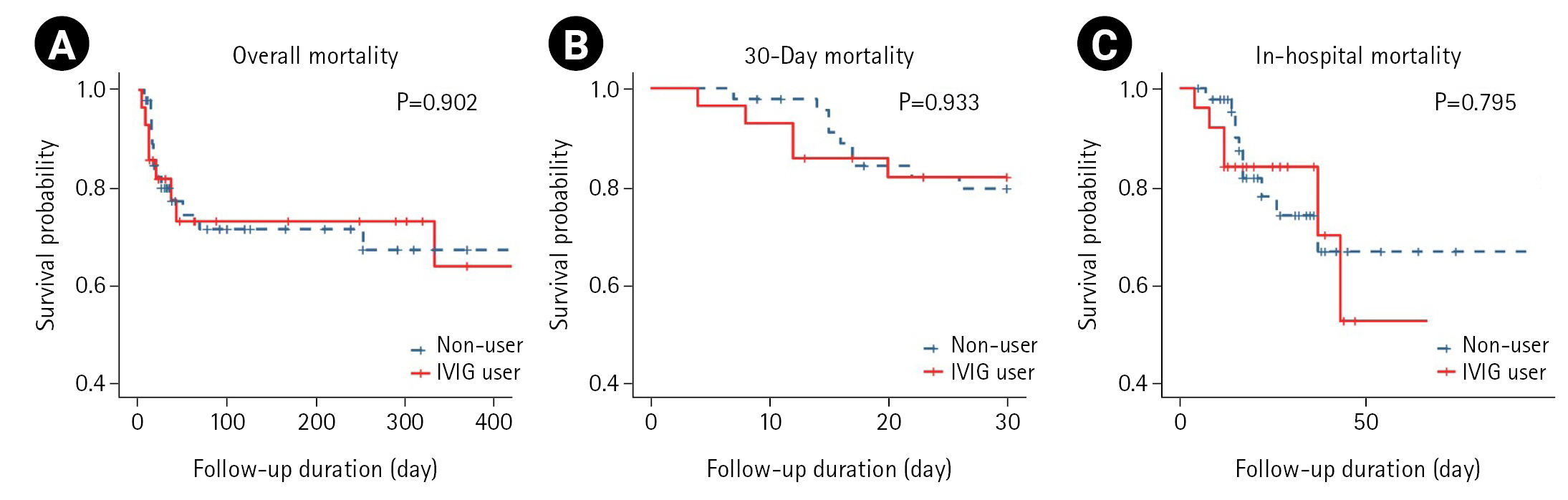
Following the propensity score matching, 28 patients were classified in the IVIG group, and 48 patients were classified in the non-IVIG group (28:48, C-statistics 0.828, Hosmer-Lemeshow test P=0.735). In the IVIG group, cancer-related perforation and DNI were high (Tables 2 and 3). In the overall population, the 30-day and in-hospital mortality rates in the IVIG group did not show better outcomes (Table 4, Figure 2). In the IVIG group, the hazard ratio for mortality and periodic indicators (ICU stay, hospital duration, and mechanical ventilator duration) showed no statistically significant difference (Table 5).
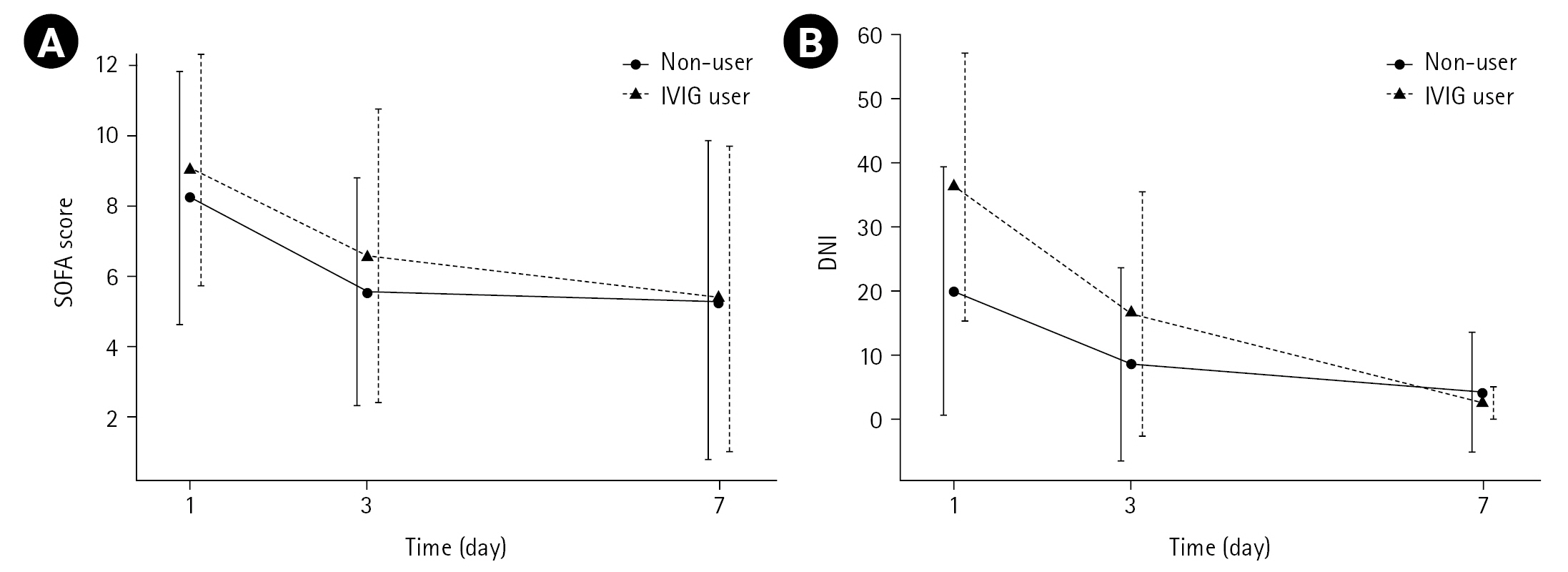
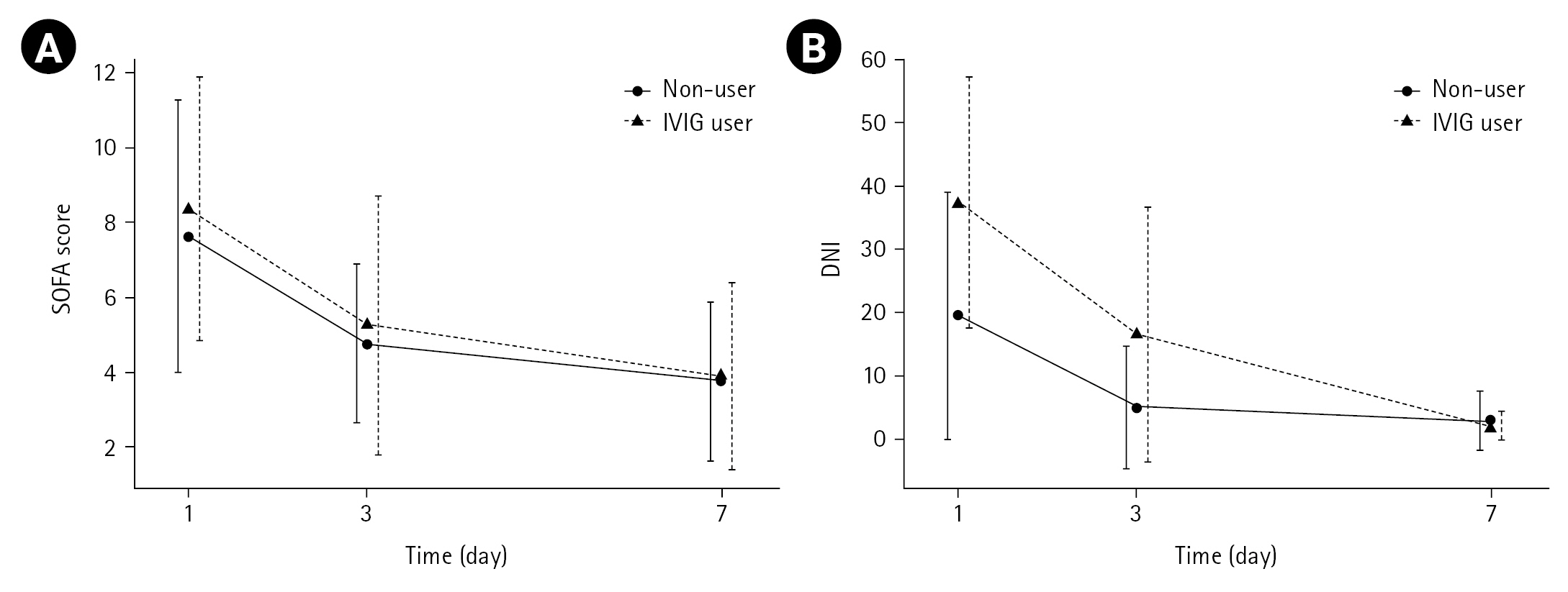
The effects of IVIG administration on SOFA and DNI changes were examined individually. For SOFA, both groups (IVIG group vs. non-IVIG group) showed a reduction, but no difference was found in the degree of change according to the use of IVIG. For DNI, the decrease was significantly greater in the IVIG group than in the non-IVIG group. As a result of confirming SOFA and DNI over time in the two groups through a linear mixed model, only time was statistically significant in SOFA, suggesting that the use of IVIG did not affect the reduction of SOFA (group×time; P=0.78). In DNI, both time and interaction terms were statistically significant (group×time; P=0.004), indicating that the reduction of DNI was faster in the IVIG group (Table 6, Figure 3). The same result was obtained when the reduction of SOFA and DNI was confirmed in surviving patients. In other words, DNI decreased faster in the IVIG group (Table 7, Figure 4).
DISCUSSION
The most important aspects in patients with secondary peritonitis are quick diagnosis, removal of the infectious source, appropriate use of antibiotics, and proper resuscitation [11]. However, despite appropriate surgery, antibiotics, and intensive care treatment, patients have shown varying outcomes. This can be explained by individuals’ unique defense mechanism, such as immunity. As mentioned in the 2016 revised definition of sepsis, which is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection, the perception of human defense mechanism to pathogens, such as the immune response, is newly becoming an important concern [10]. In recent years, immunoglobulin levels are known to decrease in septic patients, and the prognosis is generally poor [12]. In addition, interest in immunoglobulins is increasing as studies report that IVIG injections have decreased mortality in patients with sepsis [1].
Immunoglobulins exist in the serum and act as antibodies or neutralize pathogenic bacteria and viruses. Immunoglobulin injection resolves antibody deficiency caused by sepsis and stimulates the immune response against external infectious agents [13]. In multidrug-resistant gram-positive bacteria, the use of IgG enhanced the effectiveness of antibiotics, and in a meta-analysis that analyzed the effects of clindamycin in patients with streptococcal toxic shock syndrome, IVIG administration has reduced the mortality rate from 33.7% to 15.7% [8,9]. Immunoglobulin M (IgM)-rich immunoglobulins have lowered endotoxin activity in septic patients, suggesting that they may be effective in septic thrombocytopenia and fibrin deficiency [14].
In the recently published Cochrane meta-analysis, standard polyclonal IVIG and IgM-enriched polyclonal immunoglobulin (IVIgGM) were analyzed separately. In 10 studies (1,430 patients), the mortality rate between 28 and 180 days in the IVIG group was 29.6%, which was lower than 36.5% in the non-IVIG group (relative risk [RR], 0.81; 95% CI, 0.70–0.93), and in seven IVIgGM studies (528 patients), the mortality rate between 28 and 60 days was 24.7%, which was lower than 37.5% of the non-IVIG group (RR, 0.66; 95% CI, 0.51–0.85). Nevertheless, each study has multiple flaws and high heterogeneity, so the sensitivity analysis of the trials with a low risk of bias did not show a decrease in mortality, leading to an ambiguous result [6]. Two other meta-analyses showed positive results but did not show statistical significance when high-quality studies were included [15,16]. For this reason, the 2016 survival sepsis campaign does not recommend the use of IVIG in sepsis or septic shock [11].
However, IVIG treatment has differed between previous studies, such as dose of injection, duration of use, and type of immunoglobulin. Therefore, it is premature to conclude that IVIG is ineffective for sepsis based on the lack of statistical significance. Thus, the study was designed to exclude factors that could affect heterogeneity, as it was thought that heterogeneity was the reason for impending statistical significance in large-scale studies.
There are no recommendations as to when IVIG should be used, but there has been a study recommending the early use of IVIG [17]. To reflect this, the inclusion criterion of this study was restricted as the patient who used IVIG within a week after ICU admission following peritonitis surgery. As regards IVIG dose, it was followed by the Korean Health Insurance Review and Assessment Service recommends using a total of 1 mg per kg divided for 3 days. Recently, giving IVIG at a high dose is reported more effective in improving inflammation than giving IVIG at a low dose [18] , and a meta-analysis suggested that the appropriate dose of IVIG is 1.5–2 g/kg [19]). Although not intended, the dose of IVIG used in Korea is similar to the high-dose treatment or recommended dose mentioned in other studies.
AS the patient-factors and disease-severity were diverse between the two groups, propensity score matching was performed to compensate for it. Using propensity score matching, we tried to ensure that all other conditions except IVIG use were not different between the experimental group and the control group, but the DNI value was higher in the IVIG group, which is a limitation of retrospective studies. Nevertheless, there was no statistical significance in the mortality and survival curves found, but the IVIG group did not show a positive result. However, the reduction rate of DNI in the IVIG group was faster significantly than in the non-IVIG group which was an encouraging result.
DNI is a numerical value indicating the division of immature granulocyte to inflammation, is highly sensitive, and has a very fast reaction rate, which is useful for predicting the treatment process. In particular, DNI measurement has become an important prognostic indicator for the progression of sepsis as it is reported to be significantly related to the Disseminated Intravascular Coagulation score, blood culture positive rate, and mortality in sepsis patients [20,21]. In abdominal sepsis such as peritonitis, if the DNI is >7.8 within 3 days after surgery, it is reported to be more accurate than the white blood cell count, neutrophil count, and c-reactive protein level as death predictors [22]. Moreover, it has been suggested as a marker to predict MODS or 30-day mortality in appendicitis patients with complications [23] or trauma patients [24]. In this study, the initial DNI of the IVIG group was higher than that of the non-IVIG group but showed a faster rate of reduction. This means that the inflammatory response was rapidly reduced by using IVIG. Multiple organ dysfunction may affect DNI and SOFA scores when the patients are dying in the refractory phase of septic shock regardless of whether IVIG is used or not. Therefore, subgroup analysis for the reduction rates of SOFA and DNI was performed only on the surviving patients, which also showed the same result. Reduction rates of SOFA score were not different statistically between the two groups. However, reduction rates of DNI were statistically different between the two groups. The use of IVIG did not appear to affect the decrease in SOFA scores within 7 days because the SOFA score is composed of multiple factors such as consciousness status, respiratory index, and blood test results and it could also have been influenced by other factors. In this study, as DNI is a sensitive marker representing inflammation, it is thought to decrease via IVIG injection. Even though IVIG did not show improvement in mortality and hospital stay, it showed a rapid reduction of inflammation in the postoperative secondary peritonitis model.
This study has limitations as a retrospective study. In particular, the number of subjects was small and the DNI level was higher in the IVIG group. In addition, it was difficult to investigate fluid indicators and blood transfusion indicators which could be related to patient death among critically ill patients. As there were several physicians, there was a difference in the tendency to use IVIG. This is though to have influenced the results of this study. To supplement these aspects, large-scale prospective research is needed.
Due to the retrospective nature of the design, this research has limitations to adjust severity in both groups. Therefore, a prospective randomized controlled trial should be needed in the future. The use of IVIG in sepsis patients who underwent surgery for peritonitis did not show a reduction in mortality. In the group using IVIG, DNI decreased rapidly compared with the group not using IVIG. Therefore, using the IVIG for postoperative septic patients as an adjuvant therapy would be helpful for the downregulation of inflammation and it could be beneficial for the clinical outcomes of septic patients.
HIGHLIGHTS
▪ The additional use of intravenous immunoglobulin was meaningful in sepsis patients with bowel perforation after source control surgery.
▪ It was confirmed that the delta neutrophil index reduction in the use group was statistically significant compared to the control group.
NOTES
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: YUC, JYJ, KK, KSB. Data curation: JGK. Formal analysis: THG. Writing–original draft: YUC. Writing–review & editing: YUC, HS.
Acknowledgments
None.
Figure 1.Flowchart of analyzed patients. In total, 150 of 646 patients were recruited for the study. After propensity score matching, 38 were classified in the intravenous immunoglobulin (IVIG) group and 112 in the non-IVIG group, and variables were compared. ICU: intensive care unit.
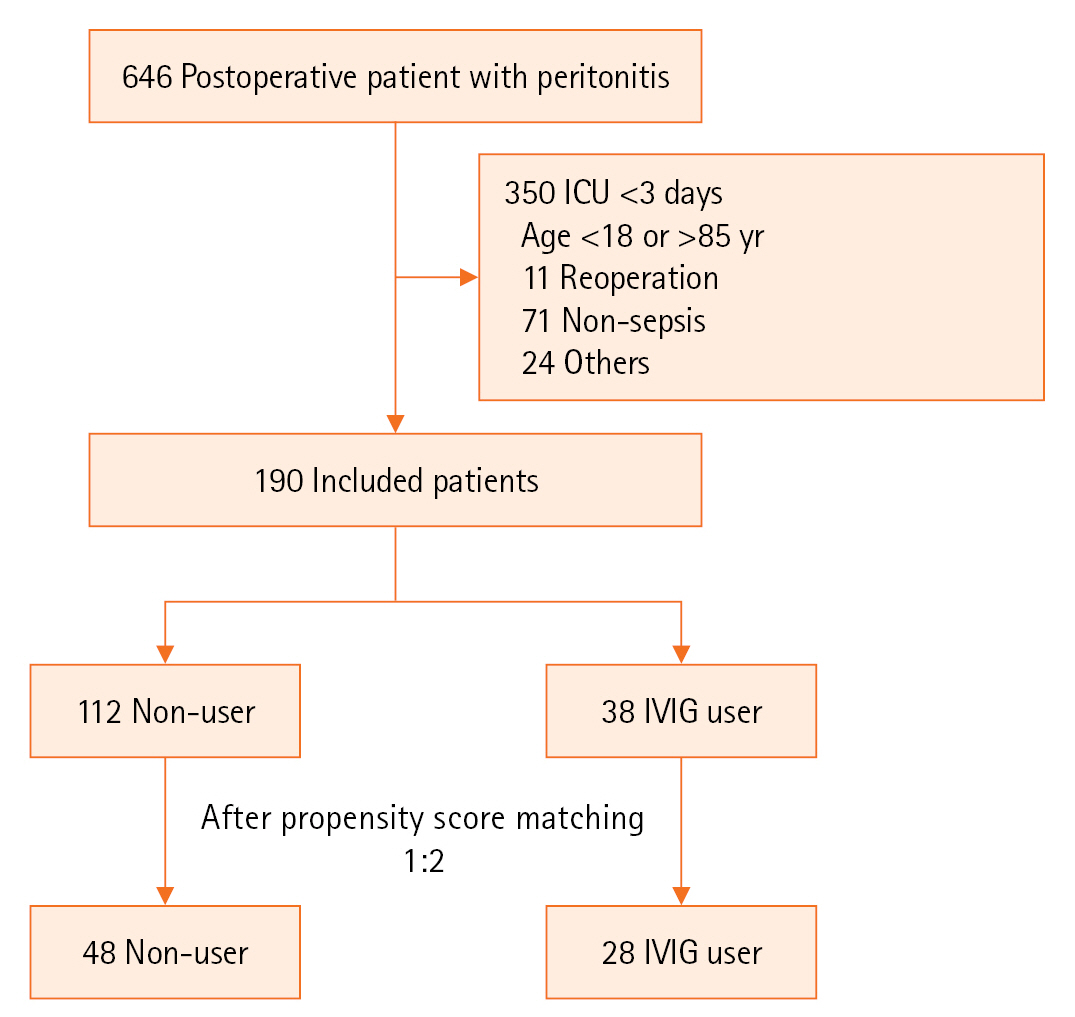
Figure 2.Survival curves of the intravenous immunoglobulin (IVIG) group and non-IVIG group. (A) Overall mortality. (B) 30-Day mortality. (C) In-hospital mortality.
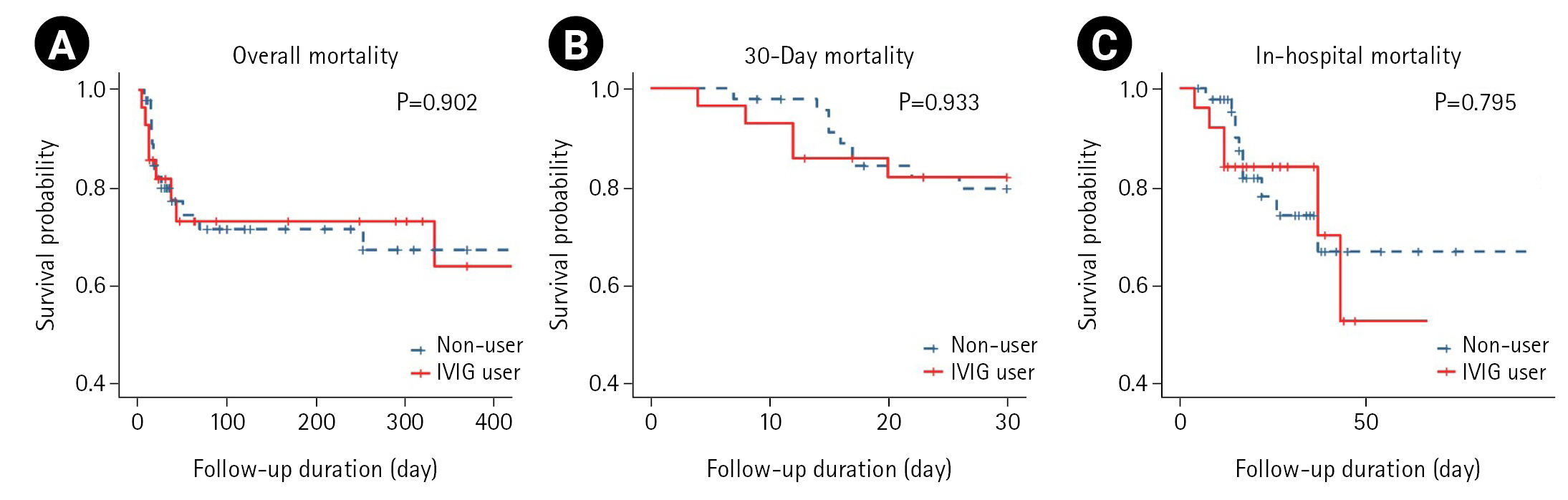
Figure 3.The change of Sequential Organ Failure Assessment (SOFA) score (A) and delta neutrophil index (DNI; B) in the intravenous immunoglobulin (IVIG) and non-IVIG groups.

Figure 4.The change of Sequential Organ Failure Assessment (SOFA) score (A) and delta neutrophil index (DNI; B) in the intravenous immunoglobulin (IVIG) and non-IVIG patients who survived.
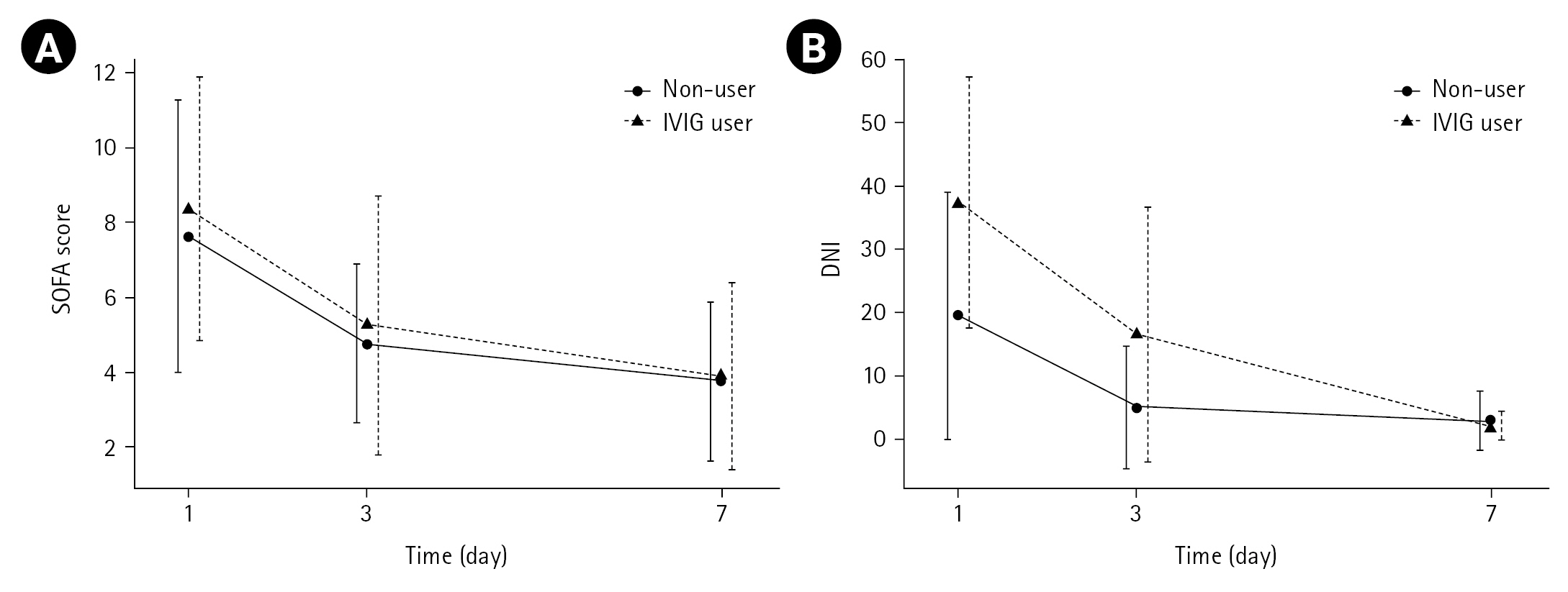
Table 1.Exclusion criteria of the study
|
Exclusion criteria |
|
Patients not met Sepsis-3 criteria |
|
Patients not given antibiotics or used properly |
|
Patients without surgery |
|
Patients undergoing reoperation |
|
Pregnant women |
|
Age <18 or >65 years |
|
Induced peritonitis patients while hospitalized due to non-surgical problem |
|
Iatrogenic chemical ingestion case for suicide |
|
Surgery was done due to suspected peritonitis but there was no specific finding |
|
Surgery was performed after more than 72 hours after onset of peritoneal symptoms |
Table 2.Baseline characteristics of patients after propensity score matching
|
Variable |
Non-user (n=48) |
IVIG user (n=28) |
Standardized difference (%) |
P-value |
|
Male, No. (%) |
29 (60.4) |
16 (57.1) |
–6.56 |
0.842 |
|
Age (yr) |
|
|
8.18 |
|
|
Mean±SD |
66.7±12.9 |
67.8±14.3 |
|
0.641 |
|
Median (range) |
73.5 (41.0 to 84.0) |
73.0 (30.0 to 82.0) |
|
0.223 |
|
Time to first antibiotics (hr) |
|
|
- |
|
|
Mean±SD |
2.2±2.2 |
1.6±1.8 |
|
0.084 |
|
Median (range) |
1.4 (0.0 to 8.3) |
1.0 (0.0 to 6.1) |
|
0.088 |
|
Time to operation after hospitalization (hr) |
|
|
–0.72 |
|
|
Mean±SD |
8.2±10.4 |
8.1±7.1 |
|
0.989 |
|
Median (range) |
5.3 (1.1 to 55.3) |
6.0 (0.2 to 32.9) |
|
0.144 |
|
Time to first IVIG after the operation (hr) |
|
|
- |
|
|
Mean±SD |
- |
2.2±5.2 |
|
- |
|
Median (range) |
- |
0.4 (–0.2 to 25.5) |
|
- |
Table 3.Outcomes of patients after propensity score matching
|
Variable |
Non-user (n=48) |
IVIG user (n=28) |
Standardized difference (%) |
P-value |
|
ICU duration (day) |
|
|
|
|
|
Mean±SD |
11.9±17.4 |
9.2±8.4 |
|
0.314 |
|
Median (range) |
7.5 (3.0 to 119.0) |
6.0 (3.0 to 36.0) |
|
0.406 |
|
Ventilator duration (day) (n=101) |
|
|
|
|
|
Mean±SD |
17.3±58.0 |
7.4±8.7 |
|
0.487 |
|
Median (range) |
4.6 (0.0 to 365.3) |
3.8 (0.3 to 35.9) |
|
0.717 |
|
CRRT |
4 (8.3) |
8 (28.6) |
|
0.052 |
|
SOFA score |
|
|
23.47 |
|
|
Mean±SD |
8.2±3.6 |
9.0±3.3 |
|
0.570 |
|
Median (range) |
8.0 (3.0 to 18.0) |
9.0 (2.0 to 15.0) |
|
0.487 |
|
APACHE Ⅱ score |
|
|
24.53 |
|
|
Mean±SD |
18.1±6.5 |
19.7±6.3 |
|
0.514 |
|
Median (range) |
18.0 (8.0 to 34.0) |
20.0 (8.0 to 36.0) |
|
0.468 |
|
BE (1 day) |
|
|
|
|
|
Mean±SD |
–7.6±4.9 |
–8.5±7.3 |
|
0.458 |
|
Median (range) |
–7.1 (–20.2 to 11.4) |
–7.9 (–28.4 to 8.3) |
|
0.296 |
|
DNI (1 day) |
|
|
|
|
|
Mean±SD |
19.9±19.4 |
36.0±20.9 |
|
<0.001 |
|
Median (range) |
11.2 (0.0 to 58.2) |
35.1 (0.0 to 79.2) |
|
<0.001 |
|
WBC (n=74) |
|
|
|
|
|
Mean±SD |
12.9±10.0 |
10.0±7.1 |
|
0.058 |
|
Median (range) |
11.6 (1.1 to 53.4) |
8.9 (2.5 to 30.0) |
|
0.062 |
|
Platelet (n=74) |
|
|
|
|
|
Mean±SD |
164.7±120.1 |
164.5±100.0 |
|
0.282 |
|
Median (range) |
132 (40 to 523) |
130 (42 to 363) |
|
0.357 |
|
Lactate |
|
|
|
|
|
Mean±SD |
3.6±3.2 |
4.2±2.6 |
|
0.356 |
|
Median (range) |
2.8 (0.3 to 13.7) |
3.1 (0.9 to 13.1) |
|
0.227 |
|
Blood culture (n=134) |
|
|
|
0.835 |
|
Positive |
23 (54.8) |
16 (57.1) |
|
|
|
Negative |
19 (45.2) |
12 (42.9) |
|
|
|
Sepsis degree |
|
|
|
0.001 |
|
Sepsis |
27 (56.3) |
6 (21.4) |
|
|
|
Septic shock |
21 (43.8) |
22 (78.6) |
|
|
|
Reason for peritonitis |
|
|
|
0.280 |
|
Gastrointestinal |
28 (59.6) |
13 (46.4) |
|
|
|
Colon |
13 (27.7) |
12 (42.9) |
|
|
|
GB related |
3 (6.4) |
1 (3.6) |
|
|
|
Others |
3 (6.4) |
2 (7.1) |
|
|
|
Comorbidity |
|
|
|
|
|
Pulmonary |
7 (14.6) |
1 (3.6) |
|
0.059 |
|
Cardiovascular |
26 (54.2) |
14 (50.0) |
|
0.532 |
|
Endocrine |
12 (25.0) |
5 (17.9) |
|
0.317 |
|
Renal |
4 (8.3) |
2 (7.1) |
|
1.000 |
|
Hepatobiliary |
0 |
1 (3.6) |
|
- |
|
Neurovascular |
4 (8.3) |
1 (3.6) |
|
0.414 |
|
Cancer perforation |
3 (6.3) |
8 (28.6) |
|
0.002 |
|
Trauma |
8 (16.7) |
1 (3.6) |
|
0.058 |
Table 4.Hazard ratios for mortality according to IVIG group and non-IVIG group
|
Outcome |
Incidence case |
Crude HR (95% CI) |
Adjusted HR (95% CI) |
|
Overall mortality |
|
|
|
|
Non-user |
13/48 (27.1) |
1.00 (Reference) |
1.00 (Reference) |
|
IVIG user |
8/28 (28.6) |
1.06 (0.44–2.55) |
1.00 (0.41–2.47) |
|
30-Day mortality |
|
|
|
|
Non-user |
9/46 (19.6) |
1.00 (Reference) |
1.00 (Reference) |
|
IVIG user |
5/28 (17.9) |
0.96 (0.32–2.85) |
1.00 (0.32–3.09) |
|
In-hospital mortality |
|
|
|
|
Non-user |
10/48 (20.8) |
1.00 (Reference) |
1.00 (Reference) |
|
IVIG user |
6/28 (21.4) |
1.14 (0.42–3.15) |
1.09 (0.38–3.15) |
Table 5.Comparison of clinical duration according to the IVIG group and non-IVIG group
|
Outcome |
Non-user (n=48) |
IVIG user (n=28) |
P-value |
|
ICU duration (day) |
|
|
|
|
Mean±SD |
11.9±17.4 |
9.2±8.4 |
0.314 |
|
Median (range) |
7.5 (3.0–119.0) |
6.0 (3.0–36.0) |
0.406 |
|
Hospital duration (day) |
|
|
|
|
Mean±SD |
30.7±29.4 |
23.0±17.5 |
0.175 |
|
Median (range) |
21.0 (5.0–152.0) |
16.0 (4.0–89.0) |
0.188 |
|
Mechanical ventilation duration (day) |
|
|
|
|
Mean±SD |
9.9±19.2 |
6.6±8.7 |
0.147 |
|
Median (range) |
5.0 (0.0–119.0) |
4.0 (0.0–36.0) |
0.012 |
Table 6.The change of SOFA score and DNI in the IVIG group and non-IVIG group
|
Day |
SOFA score
|
DNI
|
|
Non-user |
IVIG user |
P-value |
Non-user |
IVIG user |
P-value |
|
1 |
8.2±3.6 |
9.0±3.3 |
Group: 0.228 |
19.9±19.4 |
36.0±20.9 |
Group: <0.001 |
|
3 |
5.5±3.3 |
6.6±4.2 |
Time: <0.001 |
8.6±15.0 |
16.4±19.0 |
Time: <0.001 |
|
7 |
5.3±4.5 |
5.4±4.3 |
Group×time: 0.553 |
4.2±9.3 |
2.5±2.5 |
Group×time: 0.002 |
Table 7.The change of SOFA score and DNI in the survivors of the IVIG user and non-IVIG user
|
Day |
SOFA score
|
DNI
|
|
Non-user |
IVIG user |
P-value |
Non-user |
IVIG user |
P-value |
|
1 |
7.6±3.6 |
8.4±3.5 |
Group: 0.372 |
19.5±19.5 |
37.4±19.7 |
Group: <0.001 |
|
3 |
4.8±2.1 |
5.3±3.4 |
Time: <0.001 |
4.9±9.7 |
16.4±20.1 |
Time: <0.001 |
|
7 |
3.8±2.1 |
3.9±2.5 |
Group×time: 0.672 |
2.9±4.7 |
2.1±2.2 |
Group×time: 0.002 |
References
- 1. Kalvelage C, Zacharowski K, Bauhofer A, Gockel U, Adamzik M, Nierhaus A, et al. Personalized medicine with IgGAM compared with standard of care for treatment of peritonitis after infectious source control (the PEPPER trial): study protocol for a randomized controlled trial. Trials 2019;20:156. ArticlePubMedPMCPDF
- 2. Goldman DL. The other side of the coin: anti-inflammatory antibody therapy for infectious diseases. Infect Immun 2020;88:e00844-19.ArticlePubMedPMCPDF
- 3. Tamayo E, Fernández A, Almansa R, Carrasco E, Goncalves L, Heredia M, et al. Beneficial role of endogenous immunoglobulin subclasses and isotypes in septic shock. J Crit Care 2012;27:616-22.ArticlePubMed
- 4. Bermejo-Martín JF, Rodriguez-Fernandez A, Herrán-Monge R, Andaluz-Ojeda D, Muriel-Bombín A, Merino P, et al. Immunoglobulins IgG1, IgM and IgA: a synergistic team influencing survival in sepsis. J Intern Med 2014;276:404-12.ArticlePubMedPDF
- 5. Hemming VG. Use of intravenous immunoglobulins for prophylaxis or treatment of infectious diseases. Clin Diagn Lab Immunol 2001;8:859-63.ArticlePubMedPMCPDF
- 6. Sallam MM, Abou-Aisha K, El-Azizi M. A novel combination approach of human polyclonal IVIG and antibiotics against multidrug-resistant Gram-positive bacteria. Infect Drug Resist 2016;9:301-11.ArticlePubMedPMCPDF
- 7. Parks T, Wilson C, Curtis N, Norrby-Teglund A, Sriskandan S. Polyspecific intravenous immunoglobulin in clindamycin-treated patients with streptococcal toxic shock syndrome: a systematic review and meta-analysis. Clin Infect Dis 2018;67:1434-6.ArticlePubMedPMC
- 8. Alejandria MM, Lansang MA, Dans LF, Mantaring JB 3rd. Intravenous immunoglobulin for treating sepsis, severe sepsis and septic shock. Cochrane Database Syst Rev 2013;2013:CD001090. ArticlePubMedPMC
- 9. Iizuka Y, Sanui M, Sasabuchi Y, Lefor AK, Hayakawa M, Saito S, et al. Low-dose immunoglobulin G is not associated with mortality in patients with sepsis and septic shock. Crit Care 2017;21:181. ArticlePubMedPMCPDF
- 10. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017;43:304-77.PubMed
- 11. Sartelli M. Evaluation and management of abdominal sepsis. Curr Opin Crit Care 2020;26:205-11.ArticlePubMed
- 12. Bermejo-Martin JF, Giamarellos-Bourboulis EJ. Endogenous immunoglobulins and sepsis: new perspectives for guiding replacement therapies. Int J Antimicrob Agents 2015;46 Suppl 1:S25-8.ArticlePubMed
- 13. Chaigne B, Mouthon L. Mechanisms of action of intravenous immunoglobulin. Transfus Apher Sci 2017;56:45-9.ArticlePubMed
- 14. Wand S, Klages M, Kirbach C, Warszawska J, Meybohm P, Zacharowski K, et al. IgM-enriched immunoglobulin attenuates systemic endotoxin activity in early severe sepsis: a before-after cohort study. PLoS One 2016;11:e0160907. ArticlePubMedPMC
- 15. Laupland KB, Kirkpatrick AW, Delaney A. Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: a systematic review and meta-analysis. Crit Care Med 2007;35:2686-92.ArticlePubMed
- 16. Pildal J, Gøtzsche PC. Polyclonal immunoglobulin for treatment of bacterial sepsis: a systematic review. Clin Infect Dis 2004;39:38-46.ArticlePubMed
- 17. Berlot G, Vassallo MC, Busetto N, Nieto Yabar M, Istrati T, Baronio S, et al. Effects of the timing of administration of IgM- and IgA-enriched intravenous polyclonal immunoglobulins on the outcome of septic shock patients. Ann Intensive Care 2018;8:122. ArticlePubMedPMCPDF
- 18. Aubron C, Berteau F, Sparrow RL. Intravenous immunoglobulin for adjunctive treatment of severe infections in ICUs. Curr Opin Crit Care 2019;25:417-22.ArticlePubMed
- 19. Yang Y, Yu X, Zhang F, Xia Y. Evaluation of the effect of intravenous immunoglobulin dosing on mortality in patients with sepsis: a network meta-analysis. Clin Ther 2019;41:1823-38.ArticlePubMed
- 20. Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci 2008;38:241-6.PubMed
- 21. Park BH, Kang YA, Park MS, Jung WJ, Lee SH, Lee SK, et al. Delta neutrophil index as an early marker of disease severity in critically ill patients with sepsis. BMC Infect Dis 2011;11:299. ArticlePubMedPMCPDF
- 22. Kim JW, Park JH, Kim DJ, Choi WH, Cheong JC, Kim JY. The delta neutrophil index is a prognostic factor for postoperative mortality in patients with sepsis caused by peritonitis. PLoS One 2017;12:e0182325. ArticlePubMedPMC
- 23. Shin DH, Cho YS, Cho GC, Ahn HC, Park SM, Lim SW, et al. Delta neutrophil index as an early predictor of acute appendicitis and acute complicated appendicitis in adults. World J Emerg Surg 2017;12:32. ArticlePubMedPMCPDF
- 24. Kong T, Park YS, Lee HS, Kim S, Lee JW, You JS, et al. The delta neutrophil index predicts development of multiple organ dysfunction syndrome and 30-day mortality in trauma patients admitted to an intensive care unit: a retrospective analysis. Sci Rep 2018;8:17515. ArticlePubMedPMCPDF
Citations
Citations to this article as recorded by

- USING INTRAVENOUS IMMUNOGLOBULIN IN A PATIENT WITH SEPTIC SHOCK AND MULTIPLE COMORBIDITIES: A REVIEW BASED ON A CLINICAL CASE
Nataliya Matolynets, Jacek Rolinski, Khrystyna Lishchuk-Yakymovych, Yaroslav Tolstyak
Proceeding of the Shevchenko Scientific Society. Medical Sciences.2023;[Epub] CrossRef
 , Jun Gi Kim1
, Jun Gi Kim1 , Ji Young Jang2
, Ji Young Jang2 , Tae Hwa Go3
, Tae Hwa Go3 , Kwangmin Kim1
, Kwangmin Kim1 , Keum Seok Bae1
, Keum Seok Bae1 , Hongjin Shim1
, Hongjin Shim1






 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite