Mobilization phases in traumatic brain injury
Article information
Abstract
Mobilization in traumatic brain injury (TBI) have shown the improvement of length of stay, infection, long term weakness, and disability. Primary damage as a result of trauma’s direct effect (skull fracture, hematoma, contusion, laceration, and nerve damage) and secondary damage caused by trauma’s indirect effect (microvasculature damage and pro-inflammatory cytokine) result in reduced tissue perfusion and edema. These can be facilitated through mobilization, but several precautions must be recognized as mobilization itself may further deteriorate patient’s condition. Very few studies have discussed in detail regarding mobilizing patients in TBI cases. Therefore, the scope of this review covers the detail of physiological effects, guideline, precautions, and technique of mobilization in patients with TBI.
INTRODUCTION
Traumatic brain injury (TBI) has been found to be the major cause of disability and death, thus requiring admission to the intensive care unit (ICU) [1]. Many patients admitted to the ICU are viewed as immobile that may be caused by use of sedation, safety concerns, lack of teamwork, and most importantly lack of understanding regarding the role of mobilization. Prolonged immobilization may result in several detrimental effects, such as infection, increase in length of stay, and long term weakness [2]. The following could be benefited from mobilization within ICU setting in order to maintain appropriate intracranial pressure (ICP) and cerebral perfusion pressure (CPP), thus preventing from secondary brain injury [3]. Mobilization has been proven improving physical function, reduce length of stay, mechanical ventilator usage, and systemic complications [4]. Previous studies have analyzed the importance of mobilization, but few have discussed in detail regarding the steps of mobilization and when to progress mobilization in patients with TBI. Therefore, the following study emphasizes the safety of mobilization phases within ICU setting for TBI cases.
PHYSIOLOGICAL EFFECTS OF MOBILIZATION
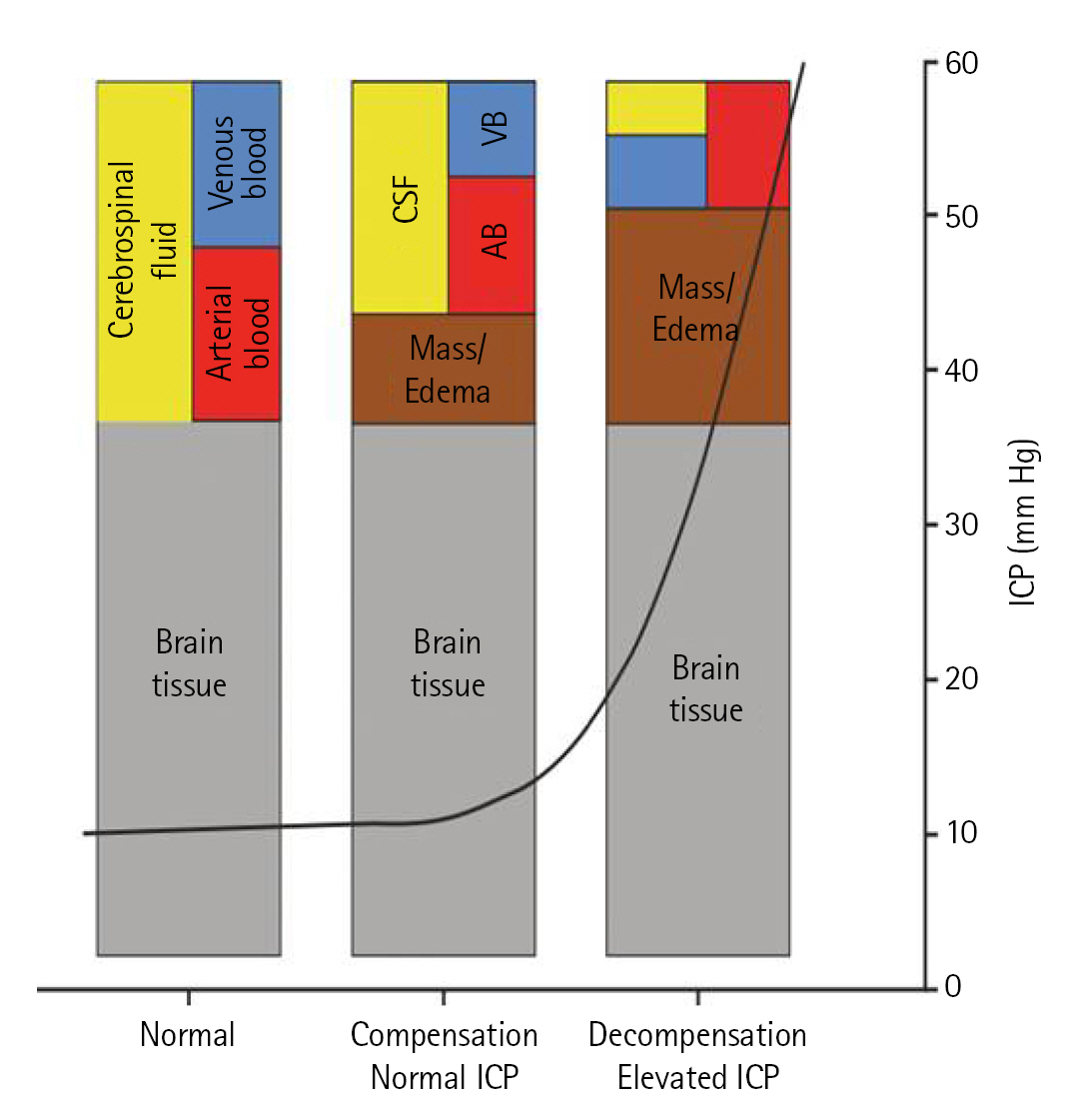
ICP is dependent on the components within the rigid skull, which includes brain (85%), blood (10%), and cerebrospinal fluid (CSF) (5%) [5]. Based on Monro-Kellie doctrine, the total amount of blood, CSF, and brain remain constant. Thus, any changes within these components would require a compensatory mechanism that would allow the total amount of pressure within the skull to remain the same (Figure 1) [6].
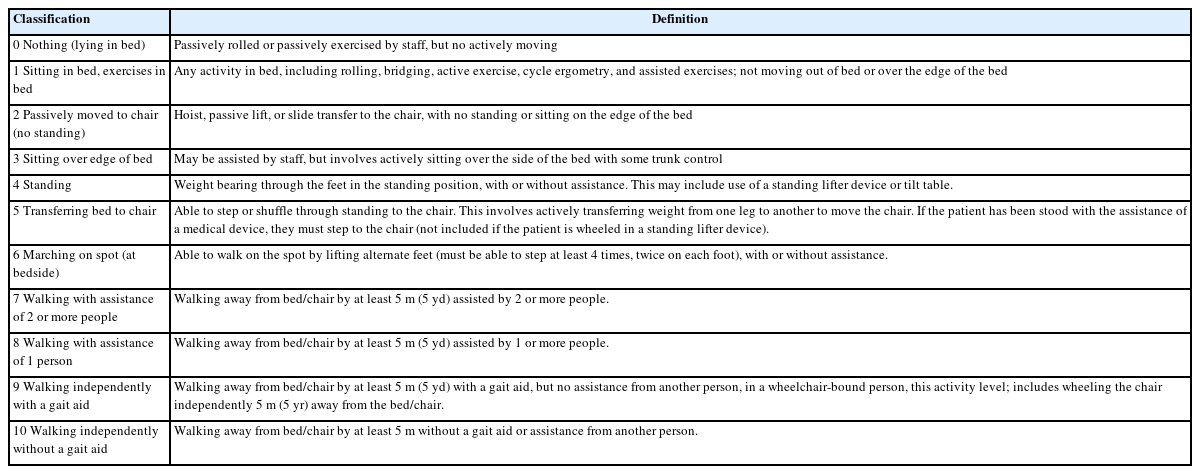
Changes of ICP can be brought by positional changes. Head up above 10°–30°, neck veins collapse with internal jugular venous pressure reaches zero, thus reducing ICP [7]. With supine or head-down tilt position, neck veins remain open and the reverse takes place during upright. Based on the study done by Chitteti et al. [8], have stated that with head of bed elevated at 15° to 30° provides best reduction in ICP and improved cerebral perfusion [8]. Sattur et al. [9] had a similar result that ICP control is benefitted with head elevation through improved venous outflow, with an addition that in severely affected brain, CPP declines with head of bed elevation beyond 30°. The following could be resulted by the dyssynchrony between several factors, such as auto regulation, compliance, head elevation, ICP pulse amplitude, CPP, and ICP. With time and evaluation of patient’s tolerance, head of bed elevation can then be further elevated [9]. As mentioned earlier, changes in ICP measurements would affect the result of CPP. Thus, with increase in degree of head position, allows greater reduction of ICP and CPP as neck veins open at a greater degree (Figure 2, Table 1) [10].
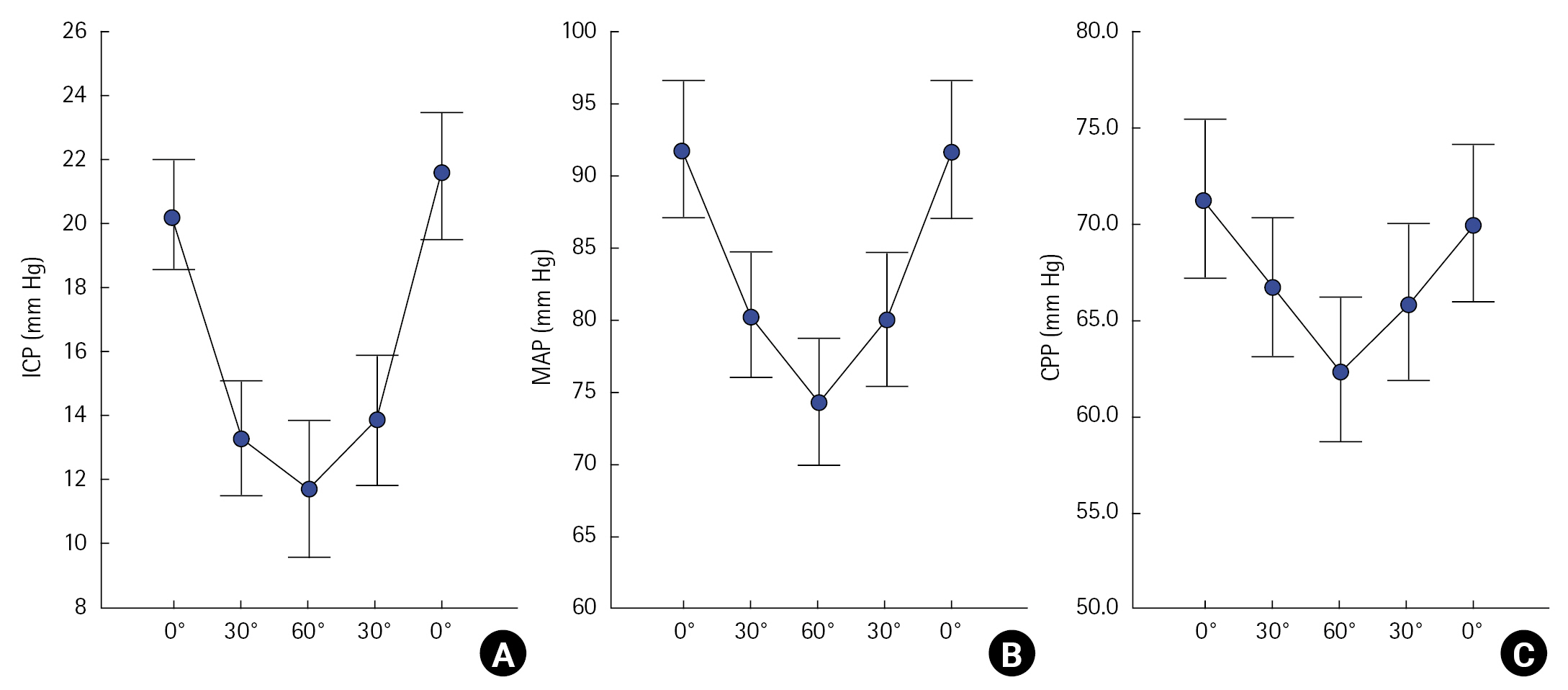
(A) Mean intracranial pressure (ICP) evaluated with head elevation from 0° to 30° and to 60°, followed by reducing head elevation from 60° to 30° and to 0°. (B) Mean arterial pressure (MAP) evaluated with head elevation from 0° to 30° and to 60°, followed by reducing head elevation from 60° to 30° and to 0°. (C) Mean cerebral perfusion pressure (CPP) evaluated with head elevation from 0° to 30° and to 60°, followed by reducing head elevation from 60° to 30° and to 0°. Adapted from Mahfoud et al. Acta Neurochir (Wien) 2010;152:443-50, with permission of Springer Nature [10].
Head of bed should be elevated by 30° as long as the patient is not hypotensive (mean arterial pressure [MAP] <60 mm Hg). Elevating the head to 30° lowers ICP via lowering cerebral and jugular venous pressures and increasing venous return, without affecting CPP, cerebral blood flow, or cardiac output appreciably. Many studies have demonstrated that shifting postures with a head elevation more than 45° results in a considerable drop in ICP. Head elevations greater than 45°, on the other hand, generally result in lower MAP and CPP. Excessive CPP reduction might result in a paradoxical rise in ICP. This demonstrates that a head elevation of more than 45° is not ideal [11].
Apart from the effects contributed by jugular venous pressure, head positioning also regulates changes within systolic blood pressure (BP). During head up position, BP lowers down due to baroreceptor relaxes, thus inducing sympathetic stimulation that will allow vasoconstriction, increased heart rate, cardiac contractility, and venous return [12]. The damage caused by TBI may result in diffuse bilateral hemisphere damage and failure of the ascending reticular activating system, which is a major factor in the manifestation of vegetative state. Meanwhile, positional changes have shown the improvement of arousal alertness [13]. Understanding these physiological changes impact greatly for healthcare workers in mobilizing patients with TBI, which would result in greater complications when not handled appropriately.
MOBILIZATION GUIDELINE IN TBI
Immobilization has been known to give rise to long term detrimental effects, which include muscle breakdown, bone resorption, cardiac and pulmonary complications, deep vein thrombosis, pulmonary embolus, and long-term cognitive and physical impairments. These effects will result in longer length of stay and the patients will also be dependent on caregiver’s assistance, within hospital nor home setting [14].
Early mobilization is known for its beneficial effects, such as improved peripheral and respiratory muscle strength, increased quality of life, earlier ventilator liberation, decreased incidence of delirium, and most importantly, greater functional independence. These includes transfer training, seated balance activity, walking, and also active or passive range of motion (ROM), thus aiming to attain independence with activities of daily living [14].
The following can be done as early as possible, commonly in critically ill patients in ICU setting, as this becomes crucial as it impacts both, in short and long term. Study done by Borges et al. [15], which includes a total of 53 patients who were involved in early mobilization despite receiving vasoactive drugs. Early mobilization may be done based on ICU mobility scale, which classifies patients' levels of mobility based on the degree of help required and the mobility milestones they have attained (Table 2) [16]. Adverse event, such as hypotension, were only observed in 1.3%. Thus, early mobilization can be safely done without facing adverse events by using the proper assessment before having mobilization [15].
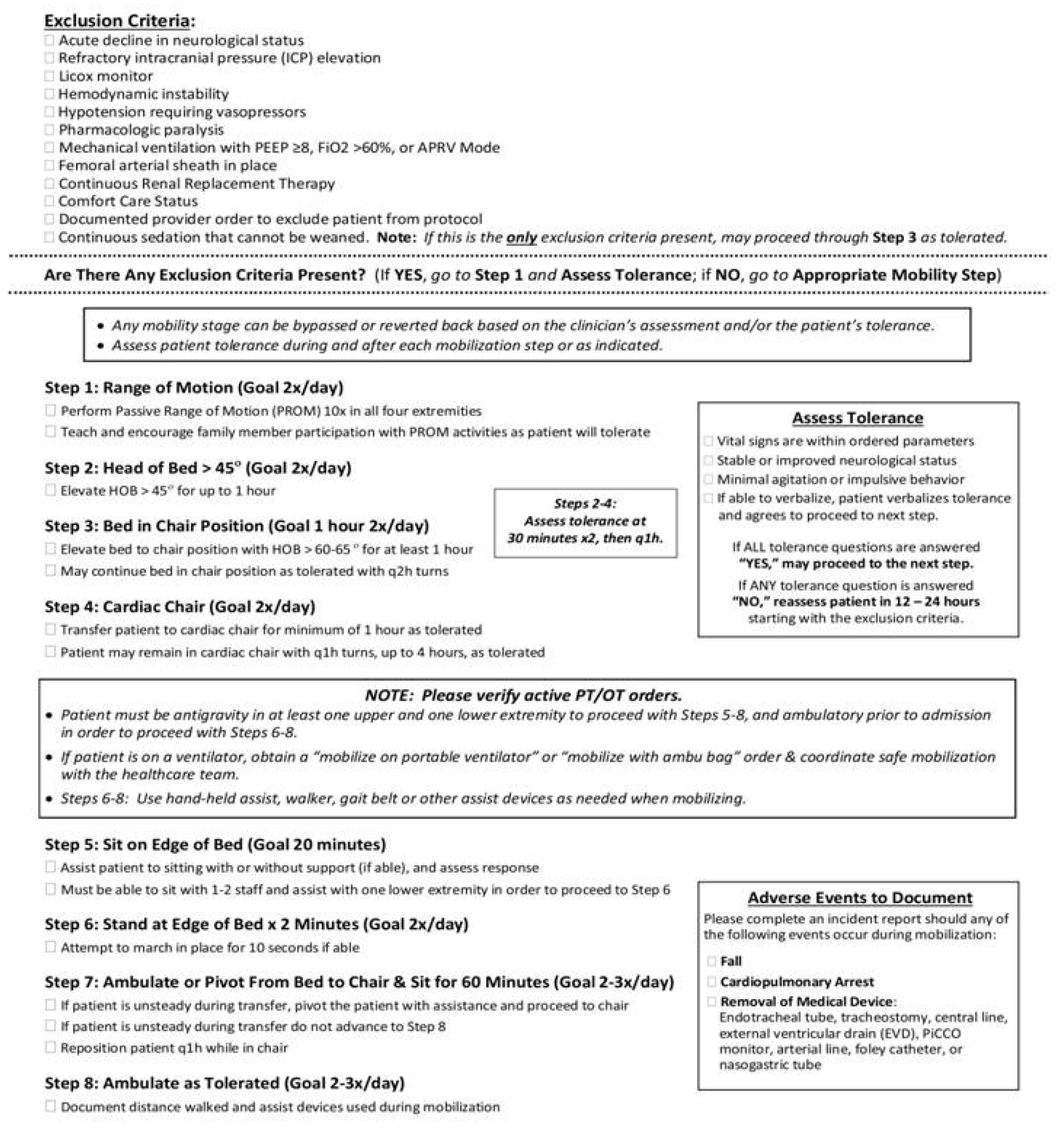
Despite its beneficial effects, the mobilization safety are not well understood by many, which may give rise to mobilization complications (fall risk and hemodynamic instability) [14]. Study analysis by Brissie et al. [2] have developed a neuro mobilization protocol (Figure 3) that may be applied within ICU setting, although it requires further study on its protocol implementation and evaluation.
Criteria for the safety of mobilization, according to Sommers et al. [17], comprise a set of red flags and relative contraindications that are crucial in ensuring safe patient mobilization. The red flags include specific parameters that need close monitoring, such as heart rate, where recent myocardial ischemia and heart rates below 40 or above 130 beats per minute are considered warning signs. BP is another critical parameter, and MAP below 60 mm Hg or above 110 mm Hg indicates potential risks during mobilization. Oxygen saturation (SpO2) levels at or below 90% serve as a cautionary measure. Parameters of ventilation, such as fractional concentration of inspired oxygen (FiO2) at or above 0.6 and positive end expiratory pressure at or above 10 cm H2O, require careful consideration. Respiratory frequency exceeding 40 breaths per minute is also considered a red flag. The level of consciousness of the patient is assessed using the Richmond Agitation Sedation Scale, and scores of –4, –5, 3, or 4 indicate potential safety concerns. High doses of inotropic drugs, including dopamine at or above 10 μg/kg/min and noradrenaline/adrenaline at or above 0.1 μg/kg/min, require special attention. Additionally, body temperature extremes of ≥38.5 °C or ≤ 36°C should be monitored closely during mobilization [17].
Apart from the red flags, relative contraindications should also be considered. These involve clinical observations, such as a decreased level of awareness/consciousness, sweating, abnormal face color, pain, and fatigue. Furthermore, conditions like unstable fractures and the presence of lines that make mobilization unsafe should be taken into account. Neurological instability, as indicated by an ICP of ≥20 cm H2O, is also considered a relative contraindication to mobilization [17]. Adherence to these safety criteria is of utmost importance in medical settings to prevent potential risks and ensure safe mobilization practices for patients with critical cardiovascular and respiratory conditions. Following these guidelines will promote patient safety and optimize the effectiveness of mobilization interventions in acute and critical care settings.
The protocol requires patient selection through several exclusion criteria, in which if any one of the criteria is present, the protocol begins at step 1 and assess tolerance. Tolerance assessment include vital signs that are within ordered parameters, stable or improved neurological status, minimal agitation or impulsive behavior, and if able to verbalize, patient verbalizes tolerance and agrees to proceed to next step. Progress may continue if all the tolerances are fulfilled and if any of them are not accomplished, then reassessment may take place within the next 12–24 hours that begins with the exclusion criteria. The exclusion criteria include: Refractory ICP elevation, Licox monitor, Hypotension requiring vasopressors, Pharmacologic paralysis, Femoral arterial sheath in place, Acute decline in neurological status, Comfort Care Status, Hemodynamic instability, Documented provider order to exclude patient from protocol, Mechanical ventilation with positive end expiratory pressure ≥8, FiO2 >60%, or airway pressure release ventilation Mode, continuous renal replacement therapy, and continuous sedation that cannot be weaned [2].
In the presence of the following red flags and/or relative contraindications, mobilization and rehabilitative treatments, such as ROM exercises, should be done passively and other active exercises will wait until patient is hemodynamically stable. As for the opposite, when the following has not been met and patient was able to follow instructions, active modalities can be prescribed, such as ROM, strengthening, and aerobic exercises (Table 3) [17].
ROM exercises should be performed with greater caution in individuals with reduced awareness. In patients who are at risk or have acquired joint contractures, may benefit from stretching exercises, splinting, or passive ROM, both manually or by the use of continuous passive motion when available that can be applied for 20 minutes. Safety requirements and degree of consciousness must be watched during the workout. Active exercise with 8–10 repetitions and 1–3 sets, as well as 20 minutes of active cycling exercise, can be administered to the patient to avoid muscle atrophy and build muscular strength [17].
The next three steps require tolerance assessment and the continued every hour. Second step is done by modifying head of bed and elevating by as much as greater than 45° for up to 1 hour twice a day. The next step requires greater mobilization, which is elevating bed to chair position with head of bed >60°–65° for at least 1 hour, and may then continue bed in chair position as tolerated with turning every 2 hours. Fourth step improves mobilization exercise by transferring patient to cardiac chair for a minimum of 1 hour as tolerated. Patient remains in the cardiac chair every hour for up to 4 hours, as tolerated [2,18].
In order to advance to the last four steps, patient must be antigravity in at least one upper and lower extremity to proceed with steps 5–8, and ambulatory prior to admission in order to proceed with steps 6–8. In ventilated patients, portable ventilator or the use of Ambu bag should be coordinated for safe ambulation. Several assistive devices, such as walker and gait belt, may be used during exercise intervention. Fifth step advances mobilization to sitting on the edge of the bed with a goal duration of 20 minutes, with or without support, and assess response. In order to move to the next step, patient must be able to sit with 1–2 staff and assist with one lower extremity. Next step requires the patient to stand at the edge of the bed for 2 minutes and repeated twice a day and if possible, to march in place for 10 seconds. In the second last step, patient can begin to ambulate or pivot from bed to chair and sit for 60 minutes, repeated 2–3 times per day. If patient is found to be unsteady during transfer, patient may pivot with assistance and proceed to chair and if patient is unsteady during transfer, it is not recommended to advance to the final step. Patient reposition every 1 hour while in chair. Final step includes ambulation as tolerance for 2–3 times per day and distance covered is measure, with or without ambulatory device [2,19].
All these steps may be bypassed or even reverted back based on assessment and/or patient’s tolerance. Tolerance assessment should be made during and after each mobilization step. During mobilization, all adverse events must be documented under several circumstances, such as fall, cardiopulmonary arrest, or removal of medical device (endotracheal tube, tracheostomy, central line, extra ventricular drain, PiCCO monitor, arterial line, foley catheter, or nasogastric tube) [2]. ICU patients must be mobilized with the help of a multidisciplinary team, including the medical staff, nursing staff, physical, occupational, and respiratory therapists, as well as speech-language pathologists. Trust that everyone is committed to keeping the patient stable and safe is necessary for this team to operate at its best.
MOBILIZATION PRECAUTIONS IN TBI
Precautions have to be understood well while mobilizing patients with TBI in order to prevent further complications. Stability for mobilization is determined by the stability of the ICP, in which normal ICP is 15 mm Hg and hemicraniectomy is initiated when ICP lies above 20 mm Hg. During mobilization, ICP is closely monitored and should be terminated when ICP exceed its limit and does not return to its normal levels within minutes. In cases where patients undergo hemicraniectomy caused by intractable brain swelling or elevated ICP, helmet should be worn. Patient’s level responsiveness should also be adjusted to intervention given to the patient. Head support may be used while sitting in a chair [20,21].
While doing mobilization intervention to patient, special attention should be made on the lines attached to the patient by preventing dislodge of catheter and over drainage of CSF. Catheter should be secured and ventriculostomy tubing should be clamped off before adjusting head position. When patient remain seated for a long period of time, CSF drainage may be resumed, as tolerated by patient’s ability to cooperate with restrictions on movement [20]. Hemiparetic patients should be positioned well, by placing the shoulder in a position that prevents shoulder subluxation. Other interventions can include the use of shoulder sling orthosis and the use of modality, such as neuromuscular electrical stimulation. In order to maximize mobilizing patients, care should also be focus on limb conditions. Any increased of muscle tone, contractures, or even edema should be managed accordingly [20].
As patient begins to mobilize out of bed, assistive device can be selected based on the amount of upper extremity control, amount of lower extremity tone, and ability to bear weight in the affected lower extremity. It is recommended to use the least restrictive ambulation device, such as walker, quad cane, or bilateral handheld support. Orthosis may also be required, such as ankle-foot orthosis, in order to stabilize foot during stance phase of walking [20]. Mobilizing prescriptions should consider several aspects, such as BP parameters, ICP, cognitive factors (level of arousal and impulsivity), logistics of tubes, drains, and equipment, and limitations on patient’s physical abilities that may be caused by paralysis or hemicraniectomy. While mobilizing, it is critical to ensure that there are no postural changes in BP by checking for orthostatic changes [20].
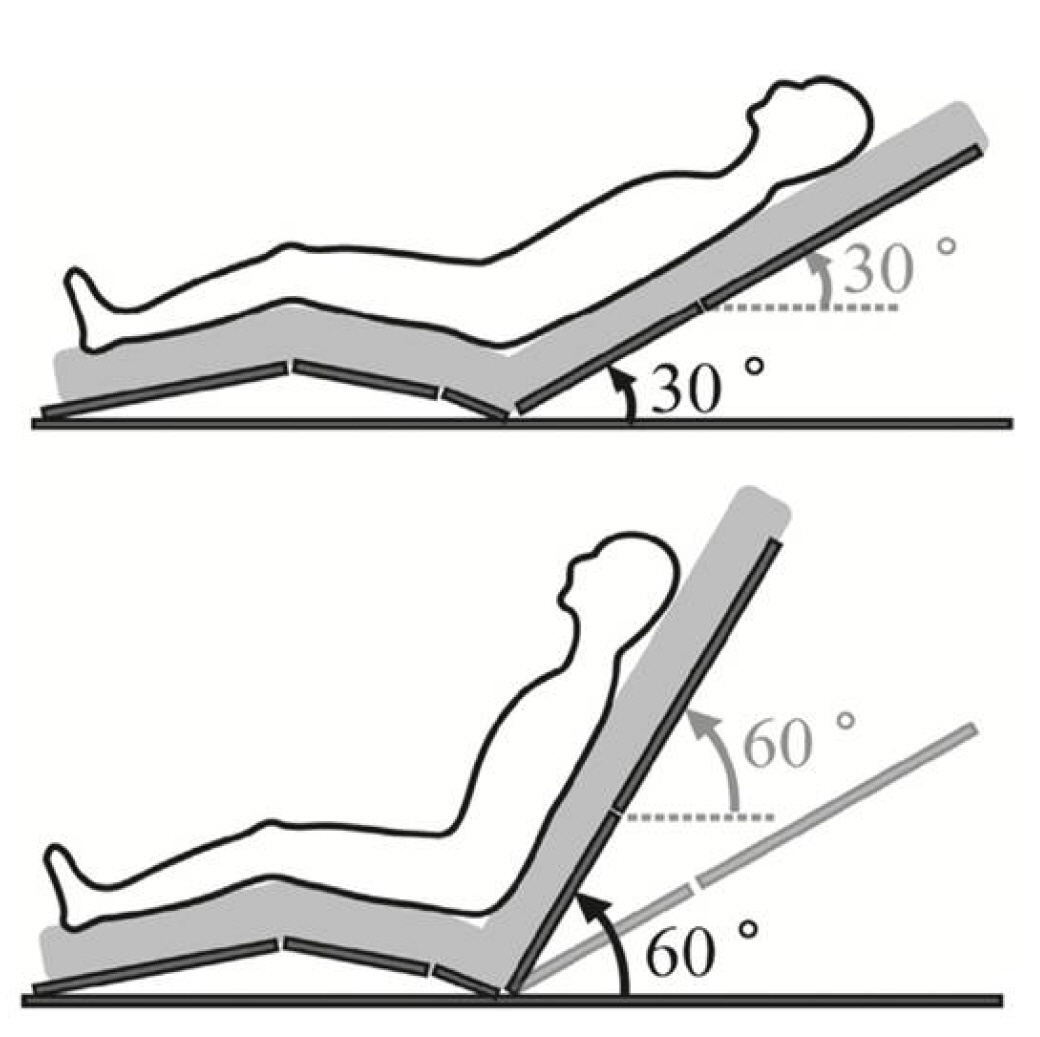
MOBILIZATION PRECAUTION IN PATIENTS WITH TBI TREATED WITH EXTRA VENTRICULAR DRAINS
Prior to beginning mobilization exercise in patients with extra ventricular drains, the physical therapist remains at the patient's bedside for at least 5 minutes in the supine position with the head of the bed elevated to 30º and the extra ventricular drains clamped, monitoring and recording heart rate, BP, and SpO2 [22]. These parameters are rigorously examined before and after each physical therapy (PT) session to look for any changes caused by the treatment. Because of the type of monitoring device available, ICP measurements were not frequently recorded. Due to the type of monitoring device available, ICP measurements were not frequently recorded. Loss of catheter, catheter malfunction, hypertension (MAP >110 mm Hg), hypotension (MAP 65 mm Hg), heart rate (40 or >130 beats per minute), SpO2 88%, vomiting, patient complaint of dizziness2or headache (7 on the visual analog scale), or nausea requiring PT termination are all considered institutional adverse events. The MAP is computed as diastolic BP+1/3 (systolic BP–diastolic BP). All such adverse occurrences are documented in electronic medical records as standard of care [4]. Figure 4 shows the head of bed elevation at 30°and 60° by Kubota et al. [22].
MOBILIZATION TECHNIQUE
In order to attain safe bed mobility, certain steps should be understood well by the caregiver. This includes safety for both the caregiver and the patient [23]. Before transferring patient, caregiver should clear the area and prepare the equipment needed that are within reach. Ensure any lines attached to the patient would not interfere during mobilization. Decide which side of the bed is best performed by the patient, based on the patient’s ability, strength and ease of transfer to chair. Position themselves to that side of the bed, in order for the patient to be able to roll towards caregiver. Adjust bed height whenever possible and required. Bed hand rails should be lowered. Providing patient education on what to expect during mobilization. Provide patient with clear directions, such as providing a countdown before starting mobilization [23]. Caregiver safety: While assisting, make sure to be as close as possible with the patient; Prevent the use of back muscles, instead always use leg muscles; Bend knees, keep back straight, and avoid back twisting to prevent any back injuries [23]. Patient safety: Avoid any movement that involves forcing or pulling the patient’s limb; Provide assistance on patient’s weaker side; Prevent any shearing force of the skin; If unsure, make sure to get help [23]. Safe steps to accomplish bed mobility: Bend patients knee furthest from the caregiver’s position; Place hands behind patient’s shoulder and hip or thigh on the far side; Roll patient towards caregiver’s side; Patient’s arm is then placed in a position that is comfortable or needed for the patient; Patient can then use the hand opposite from the bed to push the trunk in order to sit, or when assistance is needed, caregiver can support by placing one hand on the shoulder close and another can be placed on the trunk. Making sure that when transferring patient from side lying to sitting, patient needs to scoot to the edge of bed; When sitting, make sure that patient’s feet are flat on the floor and remain seated for a few seconds or minutes before leaning forward to standing position; When patient attempts to stand, have the patient lean forward, keeping both hands flat on the bed or on the lap to assist pushing off the bed from sitting to standing.
COGNITION IN TBI AND REHABILITATIVE ASPECT
Managing and treating cognitive abnormalities is one of the most difficult elements of TBI. Arousal, attention, memory, and executive control are just a few of the neuropsychological areas where cognitive issues following TBI might manifest. As they move through the rehabilitation process, patients may also display significant behavioral changes. These impairments are frequently more crippling over time than physical disability and can be closely connected to cognitive disabilities. Low frustration tolerance, agitation, disinhibition, apathy, emotional lability, mental rigidity, hostility, impulsivity, and irritability are typical behavioral sequelae [24].
Based on a systematic review research by Sharma et al. [25] that assessed six studies (with an average sample size of 42 individuals) that had fulfilled the qualifying requirements. Exercise-related benefits were observed in three investigations that employed neuroimaging and either functional or diffusion-based imaging. Although a comparable impact on cognition was not shown, the study has revealed that exercise may have a favorable impact on neuroimaging results (as measured using functional or diffusion-based imaging) following brain damage in people. The limitation to the following would be the type of exercise that allows in the improvement of cognition requires full consciousness, which is an aerobic exercise. Thus, there are limitations in improving cognitive function and requires early mobilization as an initial step to achieve higher goals.
NUTRITIONAL ISSUES IN TBI PATIENTS
Negative outcomes in critically ill patients are linked to the catabolic destruction of muscle mass and loss of functioning proteins. These are identified by significant alterations in multiple organs' hormone- and cytokine-mediated protein metabolism that result in higher rates of protein breakdown and lower rates of protein synthesis. When these conditions are left untreated, in addition with other factors, such as long-term sedation and the use of mechanical ventilation in the ICU, may result in further muscle degradation by as much as 2% of muscle mass per day, a condition known as ICU-acquired weakness may be faced In addition to targeted medication and exercise, it may be reasonable for critically ill patients to consume quantitatively more protein (compared to actual recommendations for healthy adults) to meet disease-specific increases in nitrogen/amino acid requirements and, thereby, help prevent a pronounced loss of functional proteins [26].
Currently, larger protein doses of 1.5–2.5 g/kg/day are advised for patients who are severely unwell. One hundred nineteen participants were randomly assigned to receive either 0.8 g/kg or 1.2 g/kg of protein through parenteral nutrition in the research by Mahfoud et al. [10]. They discovered a significant difference in handgrip strength at day 7 despite a smaller-than-expected difference in the protein delivery (0.9 g/kg vs. 1.1 g/kg), as well as improvements in secondary outcomes like fatigue score and measurements of the rectus femoris cross-sectional area and forearm muscle thickness [27].
Continuous feeding method may be an inappropriate method to maintain muscle structure. It has been discovered that after consuming either whey protein (45 g) or starting to receive intravenous amino acids, there is a latent period of about 30–45 minutes after which muscle protein synthesis (MPS) triples for up to 90 minutes before quickly returning to postabsorptive rates. Despite the continuous availability of necessary amino acids in the plasma and intramuscularly, MPS is reduced to its baseline level. These findings show that intermittent (bolus) eating may be preferable to continuous feeding because it may allow for the physiological stimulation of intermittent MPS [27].
Exercise and the supplementation of amino acids together have a synergistic impact on promoting MPS in healthy individuals. In the study by Zhou et al. [28], 150 patients were randomly assigned to one of three trial arms (within 48 hours of ICU admission): routine care, early mobilization, or early mobilization with early feeding. In comparison to conventional care, they found that both therapies decreased ICU-acquired weakness and increased functional status using the Barthel Index. Thus, apart from having physical activity for TBI patients, maintaining and proper management of nutrition is essential [29].
CONCLUSIONS
Mobilization intervention plays a significant role in optimizing patient recovery after TBI. Several beneficial effects contribute to an improved peripheral and respiratory muscle strength, increased quality of life, earlier ventilator weaning, decreased incidence of delirium, and greater functional independence. Basic understanding of the pathological process and mobilization effect and technique is essential, as inappropriate mobilization may result in further detrimental effects brought up by primary and secondary effects of TBI. Therefore, while mobilizing patients, precautions should always be noted, particularly ICP and hemodynamic stability, giving rise to CPP monitoring.
KEY MESSAGES
▪ Mobilization intervention plays a significant role in optimizing patient recovery after traumatic brain injury (TBI).
▪ Several beneficial effects contribute to an improved peripheral and respiratory muscle strength, increased quality of life, earlier ventilator weaning, decreased incidence of delirium, and greater functional independence.
▪ Basic understanding of the pathological process and mobilization effect and technique is essential, as inappropriate mobilization may result in further detrimental effects brought up by primary and secondary effects of TBI.
▪ Therefore, while mobilizing patients, precautions should always be noted, particularly intracranial pressure and hemodynamic stability, giving rise to cerebral perfusion pressure monitoring.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: TAN, GAP, FB, DWW. Formal analysis: TAN, IT. Data curation: IT. Visualization: IT. Writing–original draft: IT, GAP. Writing–review & editing: TAN, FB, DWW.
Acknowledgements
None.