Percent fluid overload for prediction of fluid de-escalation in critically ill patients in Saudi Arabia: a prospective observational study
Article information
Abstract
Background
Percent fluid overload greater than 5% is associated with increased mortality. The appropriate time for fluid deresuscitation depends on the patient's radiological and clinical findings. This study aimed to assess the applicability of percent fluid overload calculations for evaluating the need for fluid deresuscitation in critically ill patients.
Methods
This was a single-center, prospective, observational study of critically ill adult patients requiring intravenous fluid administration. The study's primary outcome was median percent fluid accumulation on the day of fluid deresuscitation or intensive care unit (ICU) discharge, whichever came first.
Results
A total of 388 patients was screened between August 1, 2021, and April 30, 2022. Of these, 100 with a mean age of 59.8±16.2 years were included for analysis. The mean Acute Physiology and Chronic Health Evaluation (APACHE) II score was 15.4±8.0. Sixty-one patients (61.0%) required fluid deresuscitation during their ICU stay, while 39 (39.0%) did not. Median percent fluid accumulation on the day of deresuscitation or ICU discharge was 4.5% (interquartile range [IQR], 1.7%–9.1%) and 5.2% (IQR, 2.9%–7.7%) in patients requiring deresuscitation and those who did not, respectively. Hospital mortality occurred in 25 (40.9%) of patients with deresuscitation and six (15.3%) patients who did not require it (P=0.007).
Conclusions
The percent fluid accumulation on the day of fluid deresuscitation or ICU discharge was not statistically different between patients who required fluid deresuscitation and those who did not. A larger sample size is needed to confirm these findings.
INTRODUCTION
Intravenous (IV) fluid is a common intervention in intensive care units (ICUs) [1,2]. IV fluid is often administered in large volumes in critically ill patients to improve cardiac output and ameliorate shock [3,4]. Upon hemodynamic stability, patients often receive variable amounts of fluid therapy [5]. However, IV fluid can carry significant risks to critically ill patients [6]. Fluid overload (FO) is a common complication in critically ill patients, with an incidence ranging from 30% to 70% [7-9]. FO is defined as cumulative fluid balance (FB) greater than 10% of body weight [10,11]. Positive cumulative FB has been reported in up to 40% of patients admitted to the ICU [12]; Moreover, several studies have shown that a persistent cumulative positive FB negatively impacts ICU patient outcomes [2,13]. In patients with acute lung injury, positive FB was associated with further impaired oxygenation and prolonged need for mechanical ventilation [11,14]. On the other hand, negative FB has been advocated for as an indication of early cessation of mechanical ventilation [6]. Some observational studies have reported negative FB to be associated with lower risk-adjusted short-term mortality compared to patients with positive FB [12].
The term deresuscitation or de-escalation was first suggested in 2012, and finally coined in the literature in 2014 [13]. Deresuscitation or de-escalation refers to the phase of critical illness after initial resuscitation, stabilization, and optimization [15]. Deresuscitation is widely practiced mitigating the potential harm of FO. The active deresuscitation phase is initiated when FO is clinically identified and hemodynamic stability has been attained and should be assessed daily [16].
Information about the appropriate timing of fluid deresuscitation mainly depends on physician assessment of patient clinical and radiological findings. Historically, many studies have found a relationship between calculated percent FO greater than 5% and mortality [10,12,17]. However, none of the studies evaluated the relationship between percent FO and need for fluid deresuscitation. Therefore, our study aimed to assess the applicability of percent FO calculation for evaluating the need for fluid deresuscitation by diuretics and/or renal replacement therapy (RRT) in critically ill patients.
MATERIALS AND METHODS
Ethics Approval and Consent to Participate
A single-center, prospective, observational study was conducted between August 01, 2021, and April 30, 2022. The study was approved by the King Faisal Specialist Hospital and Research Center Institutional Review Board, Jeddah, Saudi Arabia (No. 2021-19). To ensure patient privacy and confidentiality, limited data access was available to study investigators. Informed consent from study participants was waived by the board due to the study's observational nature. The study was conducted in accordance with local regulations, and ethical principles were ensured in accordance with the Declaration of Helsinki.
Patients
Enrollment criteria include patients 18 years old or older who were admitted to the medical ICU and IV fluids, including colloids and/or crystalloids, as a replacement or resuscitation. Exclusion criteria were age <18 years, end-stage renal disease, on hemodialysis, on diuretics upon ICU admission, on maintenance IV fluids >72 hours before ICU admission, started on RRT 24 hours post-ICU admission, on the diabetic ketoacidosis or hyperosmolar hyperglycemic state protocol, or inability to measure fluid output (Supplementary Figure 1).
Data Collection
Data screening occurred each Sunday, excluding holidays. All patients who fulfilled the criteria were considered for inclusion. Patients were followed until the day of deresuscitation by diuretics, RRT, or ICU discharge, whichever came first. The total amount of fluid administered including IV resuscitation fluids, IV maintenance fluid, IV medications, and total parenteral nutrition was calculated every 24 hours until deresuscitation or ICU discharge. We also collected information on comorbidities, severity scores, acute kidney injury, use of mechanical ventilation (MV), and FB. Patient data were collected and handled using Research Electronic Data Capture (REDCap) software.
Outcomes
This study's primary outcome of interest is the median percent fluid accumulation on the day of fluid deresuscitation or ICU discharge, whichever comes first. Secondary outcomes were median FB at 24, 48, and 72 hours of ICU stay; duration of mechanical ventilation; length of hospital and ICU stays; and ICU and hospital mortality. Primary exposures of interest were Acute Physiology and Chronic Health Evaluation (APACHE) II score, diagnosis of acute respiratory distress syndrome (ARDS) upon ICU admission and need for mechanical ventilation. Other characteristics of interest were age, gender, weight, body mass index, source of ICU admission, other ICU admission diagnoses, comorbidities, need for vasopressors, use of nephrotoxic drugs, and whether a Foley catheter was removed before ICU discharge or starting diuretics or RRT.
Definitions
Percent FO was defined as the total cumulative FB in liters from ICU admission to the first of fluid deresuscitation or ICU discharge divided by patient baseline weight upon hospital admission, multiplied by 100 [11]. Our study calculated percent FO only for patients with positive FB at deresuscitation. Fluid deresuscitation or de-escalation is defined as active fluid removal through diuretics and RRT with net ultrafiltration [15].
Sample Size and Statistical Analysis
No previous studies have investigated percent FO as a primary outcome. For this reason, am adequate sample size could not be estimated. All patients who fulfilled the inclusion criteria during the study period were enrolled. The normality of the continuous predictor variables was assessed using Shapiro-Wilk and Kolmogorov-Smirnov tests by comparing median and mean values and observing the data graphically. The associations between exposure variables, baseline and clinical characteristics, and fluid deresuscitation status were assessed using Student t-test, Wilcoxon two-sample test with normal approximation, chi-square test, and Fisher's Exact Test. The associations between predictor variables and hospital mortality also were assessed using these bivariate tests, as were the associations between patient fluid and mortality outcomes by fluid deresuscitation status. Fluid outcomes were also evaluated at 24-, 48-, and 72-hour post-ICU discharge. A multivariable logistic model adjusted for age, APACHE Ⅱ score, deresuscitation status, ARDS, and need for MV at baseline was constructed to examine the associations between the primary exposures of interest and hospital mortality. Analyses were performed using SAS analytics software ver. 9.4 (SAS Institute), and statistical significance was determined at an α=0.05 level.
RESULTS
The study population included 100 ICU patients with a mean age of 59.8 years and a male proportion of 57.0%. A total of 57.0% of the patients required mechanical ventilation (Table 1), and 61.0% of the patients underwent fluid deresuscitation with either diuretic, RRT, or both. Specifically, 59% of patients received diuretics, while 18.0% underwent RRT (Supplementary Table 1). The median time from ICU admission to diuretic therapy was 2.0 days (interquartile range [IQR], 1.0–4.0), and the median time from ICU admission to RRT was 4.0 days (IQR, 2.0–9.0) (Supplementary Table 1).
The patients who received fluid deresuscitation were significantly older, with a mean age of 62.5 years, compared to patients who did not receive fluid deresuscitation, with a mean age of 55.6 years (P=0.036) (Table 1). The mean APACHE II score was also significantly higher for patients that received fluid deresuscitation compared to those who did not (17.2 vs. 12.4, P=0.003). The association between ICU admission diagnosis of ARDS and need for fluid deresuscitation was significant, with 92.3% of the patients diagnosed with ARDS requiring fluid deresuscitation compared to 7.7% of ARDS patients not needing fluid de-resuscitation (P=0.014) (Table 1).
Median percent fluid accumulation on the day of deresuscitation or ICU discharge was 4.5% (IQR, 1.7%–9.1%) and 5.2% (IQR, 2.9%–7.7%) in patients who required deresuscitation and those who did not, respectively (P=0.723). The median total fluid intake on the day of ICU discharge was significantly higher among patients that did not receive fluid deresuscitation (7,029.5 ml; IQR, 4,904.6–9,354.0 ml) compared to patients that did (5,274.8 ml; IQR, 2,580.5–8,862.8 ml) (P=0.049) (Table 2). Indeed, fluid intake and total fluid cumulative balance varied based on the time of deresucetation (Supplementary Table 2). ICU length of stay was 16.3 (IQR, 8.0–24.1) vs. 2.35 (IQR, 0.8–7.4) days (P<0.001), and hospital length of stay was 25.4 (IQR, 15.5–54.9) vs. 8.4 (IQR, 5.8–17.6) days (P<0.001) (Table 2). A total of 31 patients (31.0%) experienced hospital mortality in our cohort (Supplementary Table 3).
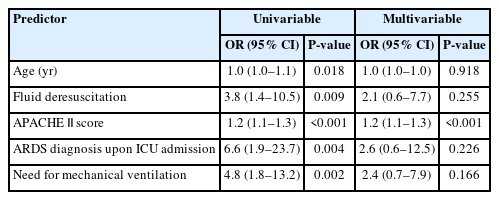
In the multivariable model controlling for the main exposure variables, higher APACHE II score was associated with increased likelihood of hospital mortality, and patients were 20% more likely to die in the hospital with every one-unit increase in score (adjusted odds ratio, 1.2; 95% confidence interval [CI], 1.1–1.3; P<0.001) (Table 3).
DISCUSSION
This single-center, observational study was conducted to assess the applicability of percent FO calculation for evaluating the need for fluid deresuscitation in critically ill patients. Many studies have used percent FO calculation as a cutoff to define FO or fluid accumulation [10,11,17].
Our study found no statistically significant differences in median percent fluid accumulation on the day of deresuscitation or ICU discharge in patients who did not require fluid deresuscitation, with a value of 5.2% (2.9%–7.7%) compared to the 4.5% (1.7%–9.1%) in patients who received deresuscitation of fluid (P=0.723). However, the median total volume of fluid administered was significantly higher in patients in the no deresuscitation arm (7,029.5 ml; IQR, 4,904.6–9,354.0 ml) than in the deresuscitation arm (5,274.8 ml; IQR, 2,570.5–8,862.8 ml) (P=0.049). These findings can explain the lack of relationship among amount of fluid administered, percent fluid accumulation, and need for fluid deresuscitation.
Several studies have demonstrated an association of percent FO with mortality [10,11,17]. Our study showed that mortality was significantly higher in patients who required fluid deresuscitation than in those who did not (ICU mortality: 34.4% vs. 12.8%; P=0.016) and hospital mortality (40.9% vs. 15.3%; P=0.007). This is explained by the higher mean APACHE II score in the patients who required fluid deresuscitation during their ICU stay, representing the sicker group (17.2±7.1 and 12.4±8.6; P=0.003). In the multivariable logistic model, APACHE II score was a significant predictor of hospital mortality (OR, 1.2; 95% CI, 1.1–1.3). On the other hand, a recent study found a significant reduction in ICU length of stay (mean difference, –1.88 days; 95% CI, –0.12 to –3.64) with de-resuscitative strategies compared to the standard approach [3]. In our observational study, lengths of stay in the ICU and in the hospital overall were significantly longer for sicker patients requiring fluid deresuscitation.
In our study, 18% of the patients presented with septic shock. Approximately 55% of patients required fluid deresuscitation during their ICU stay. Positive FB in patients with sepsis was associated with poor 28-day survival and with increased 60-day survival of patients with acute renal failure [7]. A retrospective study that investigated fluid administration in early sepsis and septic shock found that administration of more than 5 L of fluid on the first day of shock was associated with increased mortality [18]. Subsequent studies have proposed that "fluid accumulation" or "positive fluid balance” in septic patients is mainly related to the severity of illness and is a marker of poor outcome [19,20]. However, the recent Restriction of Intravenous Fluid in ICU Patients with Septic Shock (CLASSIC) study randomized 1,554 patients with septic shock to a fluid restrictive or standard care protocol. The study did not find a mortality benefit of a fluid restriction strategy in sepsis [21].
The duration of mechanical ventilation is a crucial outcome of interest in fluid studies. In a systematic review and meta-analysis of the restrictive fluid approach in adult patients with septic shock, a longer duration of ventilator-free days was observed with the de-resuscitate strategy [22]. However, in the Role of Active Deresuscitation After Resuscitation-2 (RADAR-2) study, no significant difference in ventilator-free days was found among critically ill patients who underwent active fluid deresuscitation compared with usual care [3]. In our observational study, mechanical ventilation days were higher in number in the sicker group who required fluid deresuscitation by either diuretics or RRT (median, 9 days; IQR, 5.0–15.0 vs. 4 days, 1.0–8.0; P=0.004).
The patients included in our analysis broadly represent those treated in the ICU and reflect real-world practice. Our study was the first to describe the average range of percent FO that required deresuscitation in critically ill patients. However, it had several limitations, including the observational nature, the small sample size, and the lack of study power. In addition, the difference in baseline APACHE II scores between the two comparative arms might have affected the outcome. The study did not investigate the number of blood transfusions administered to patients, the amount of fluid removed during the dialysis sessions, or the clinician reported reason for fluid deresuscitation. Future studies are warranted to guide the appropriate timing for fluid de-resuscitation among critically ill patients using specific clinical and radiological criteria. Moreover, larger studies testing the possibility of percent overload calculations as a guide for the need for fluid de-resuscitation or a tool for patient fluid assessment are needed.
In conclusion, our observational study found that percent fluid accumulation calculation on the day of deresuscitation or ICU discharge was not significantly different between patients requiring fluid deresuscitation and those who did not. Thus, percent FO cannot be considered as a predictive tool for fluid deresuscitation. A study with a larger sample size is needed to confirm these findings.
KEY MESSAGES
▪ This study aimed to assess the applicability of the percent fluid overload calculation along with clinical and radiological assessment to evaluate the need for fluid deresuscitation in critically ill patients.
▪ The study did not find a significant relationship between percent fluid overload and need for fluid deresuscitation.
▪ Our study suggested a cutoff value of percent fluid overload that requires fluid deresuscitation among critically ill patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: HH, NFA. Methodology: HH, NFA. Formal analysis: ELGH. Data curation: RAA, AHA, AMA, NFA. Visualization: NFA. Project administration: NFA. Writing–original draft: RAA, NFA. Writing–review & editing: NFA.
Acknowledgements
None.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4266/acc.2022.01550.
Characteristics of patient’s fluid deresuscitation outcome
acc-2022-01550-Supplementary-Table-1.pdfPatient outcomes by fluid deresuscitation at 24 hours, 48 hours, and 72 hours
acc-2022-01550-Supplementary-Table-2.pdfClinical characteristics for all patients by hospital mortality
acc-2022-01550-Supplementary-Table-3.pdfFlow diagram showing patients recruitment.
acc-2022-01550-Supplementary-Fig-1.pdf