Clinical efficacy of blood purification using a polymethylmethacrylate hemofilter for the treatment of severe acute pancreatitis
Article information
Abstract
Background
Severe acute pancreatitis (SAP) is a systemic inflammatory disease, and it can often complicate into acute kidney injury (AKI) and acute lung injury/acute respiratory distress syndrome (ALI/ARDS). This study aimed to evaluate the clinical effectiveness of blood purification using a polymethylmethacrylate (PMMA) hemofilter.
Methods
We retrospectively examined 54 patients, who were diagnosed with SAP according to the Japanese criteria from January 2011 to December 2019.
Results
Of a total of 54 SAP patients, 26 patients progressively developed AKI and required continuous hemodialysis with a PMMA membrane hemofilter (PMMA-CHD). Acute Physiology and Chronic Health Evaluation (APACHE) II score and Sequential Organ Failure Assessment (SOFA) score were significantly higher in patients requiring PMMA-CHD than in patients not requiring hemodialysis. The lung injury scores were also significantly higher in patients requiring PMMA-CHD. Of the 26 patients, 16 patients developed ALI/ARDS and required mechanical ventilation. A total of seven patients developed severe ALI/ARDS and received additional intermittent hemodiafiltration using a PMMA hemofilter (PMMA-HDF). Although the length of intensive care unit stay was significantly longer in patients with severe ALI/ARDS, blood purification therapy was discontinued in all the patients. The survival rates at the time of discharge were 92.3% and 92.9% in patients with and without PMMA-CHD, respectively. These real mortality ratios were obviously lower than the estimated mortality ratios predicted by APACHE II scores.
Conclusions
These finding suggest that the blood purification using a PMMA hemofilter would be effective for the treatment of AKI and ALI/ARDS in SAP patients.
INTRODUCTION
Acute pancreatitis (AP) is a common gastrointestinal disease, and the majority of AP patients usually experience a mild course of disease. However, in approximately 20% of AP patients, damage to the tissue around the pancreatitis could worsen further, resulting in deterioration with multiple organ failure (MOF) and subsequent diagnosis of severe AP (SAP), particularly hampering the kidney and pulmonary functions [1,2]. If acute kidney injury (AKI) develops, the mortality of SAP patients increases to between 20% and 80% [2,3]. More recent publications have reported a decrease in the mortality of AP patients with AKI over the past decade; however, AKI is still independently associated with higher mortality [4]. As in other critically ill patients with AKI, renal replacement therapy is indicated as a treatment method in such cases [5].Acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) is also known as a major complication of SAP and has been reportedly associated with an increased mortality of up to 50% [6].
Although blood purification therapy is still not a standard therapy for SAP, continuous blood purification therapy using a polymethylmethacrylate (PMMA) hemofilter is used as a potential treatment method for SAP in Japan. A hemofilter made from a PMMA hollow-fiber membrane is reportedly capable of efficiently removing the proinflammatory mediators from the blood through adsorption [7,8]. It shows a positive effect on patients with systemic inflammatory response syndrome (SIRS), such as septic shock, ARDS, and SAP [9-11]. This study aimed to present our clinical experience of the last 9 years of managing SAP patients requiring continuous hemodialysis with a PMMA membrane hemofilter (PMMA-CHD) and to evaluate the improvement in organ failures of AKI and/or ALI/ARDS and treatment outcomes.
MATERIALS and METHODS
Study Design, Patients, and Treatments
This study was approved by the Ethical Committee of Okinawa Kyodo Hospital. And informed consent was obtained from all patients. We retrospectively reviewed a total of 54 patients who were diagnosed with SAP according to the Japanese severity criteria for AP of the Japanese Ministry of Health, Labour, and Welfare [12] and were admitted to the intensive care unit (ICU) between January 1, 2011, and December 31, 2019. According to the Japanese criteria, SAP was determined as grade 2 or 3 of pancreatic tissue involvement evaluated by contrast-enhanced computed tomography (CT) with optional evaluation by prognostic factors [12]. Initially, for these patients were treated with conventional therapy, including massive infusion and administration of diuretics, antibiotics, and multi-enzymatic protease inhibitors, according to Japanese guidelines for the management of SAP [13]. Nevertheless, when patients had anuria or oliguria with <200 ml urine output during the initial 8–12 hours of ICU stay, they were treated with PMMA-CHD, as described below. During treatment with PMMA-CHD, diuretic administration was continued. If patients developed ALI/ARDS with further systemic deterioration, high-flow-volume hemodiafiltration (HDF) using a 2.1-m2 PMMA hemofilter was intermittently used between sessions of PMMA-CHD. Blood purification therapies were discontinued when both AKI and ALI/ARDS improved, defined as improved oliguria (urine output >600 ml/day) and a PaO2/FiO2 ratio of >400 or extubation in patients in the ventilation group.
Blood Purification Therapy
A double-lumen catheter was inserted in the cervical or femoral vein for blood access. ACH-Σ (Asahi-Kasei, Tokyo, Japan) was used for continuous hemodialysis. Continuous hemodialysis was initiated using a 1.3-m2 PMMA hemofilter (Hemofeel CH-1.3W; Toray, Tokyo, Japan). The blood flow rate was set at 80 ml/min, and the flow rate of dialysate was set at 600 ml/hr. The hemofilter was exchanged every 24–48 hours. Nafamostat mesilate (Torii Pharmaceutical, Tokyo, Japan), a synthetic serine protease inhibitor, was used as an anticoagulant. From the second or third day of ICU stay, a large-sized (1.8 m2) PMMA hemofilter (Hemofeel CH-1.8W, Toray) was used. For further deteriorated patients, intermittent PMMA-HDF was used for 6 hours between interrupted PMMA-CHD sessions, according to the procedure described by Nishida et al. [14], with some modifications as follows: a 2.1-m2 hemofilter (NF-2.1H, Toray) was used. The blood flow rate was set at 80–120 ml/min, the flow of dialysate was set at 300 ml/min, and the filtration rate was set at 1,000 ml/hr using a HDF equipment, NDF-21 (Nipro, Tokyo, Japan). A setup of blood purification system is shown in Figure 1.
Evaluation of the Severity of Patient Conditions
Acute Physiology and Chronic Health Evaluation (APACHE) II scores were used to evaluate the severity of patients before initiating the blood purification therapy in the ICU [15]. Sequential Organ Failure Assessment (SOFA) scores were used to assess the severity of organ failures during the clinical course in the ICU [16]. The pancreas and/or surrounding tissues were classified based on the Balthazar CT severity index (CTSI) [17]. Acute renal failure was classified based on the Kidney Disease: Improving Global Outcome (KDIGO) stage [18]. Acute respiratory failure due to ALI/ARDS was assessed using the lung injury score (LIS) [19]. SOFA score, KDIGO stage and LIS were recorded before and after using the PMMA-CHD.
Statistical Analysis
Data are presented as mean±standard deviation. Categorical variables were analyzed using the Fisher’s exact test. The Wilcoxon rank-sum test was used for two-group comparison. Statistical software (JMP ver. 14; SAS Institute, Cary, NC, USA) was used for these analyses. Significant differences between groups were decided at P<0.05.
RESULTS
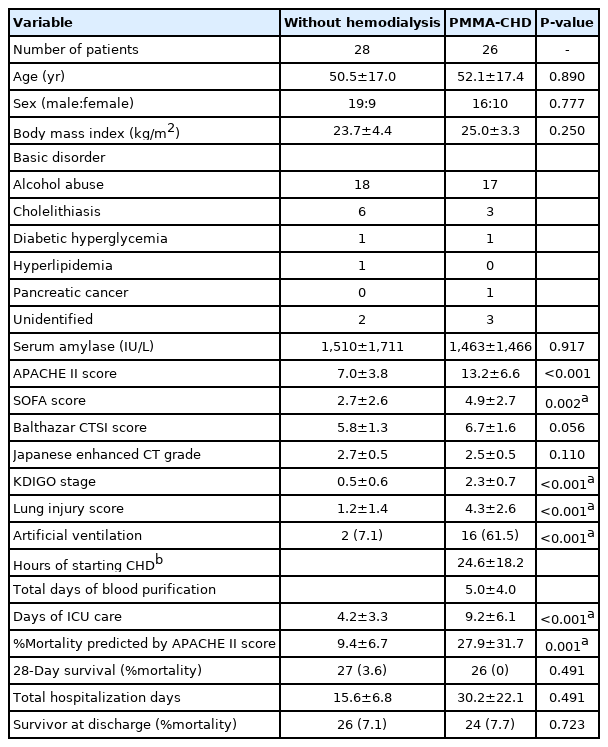
Among 54 SAP patients, 26 patients progressively developed anuria or oliguria during the initial 8–12 hours of ICU stay and were treated with PMMA-CHD (PMMA-CHD group) (Figure 2). The baseline characteristics of all 54 patients are summarized in Table 1. No significant differences were noted in the age, sex, body mass index, etiology, Japanese grade evaluated with contrast-enhanced CT, and Balthazar CTSI between the PMMA-CHD and non-hemodialysis groups. The serum amylase levels were remarkably high in both the groups. AKI was significantly more severe in patients in the PMMA-CHD group than in those in the non-hemodialysis group, as per the KDIGO stage at admission. The APACHE II and SOFA scores were also significantly higher in patients requiring PMMA-CHD (Table 1). The LIS of the patients in the PMMA-CHD group was significantly higher than that of patients in the non-hemodialysis group. The final survival ratio showed no significant difference between these two groups.
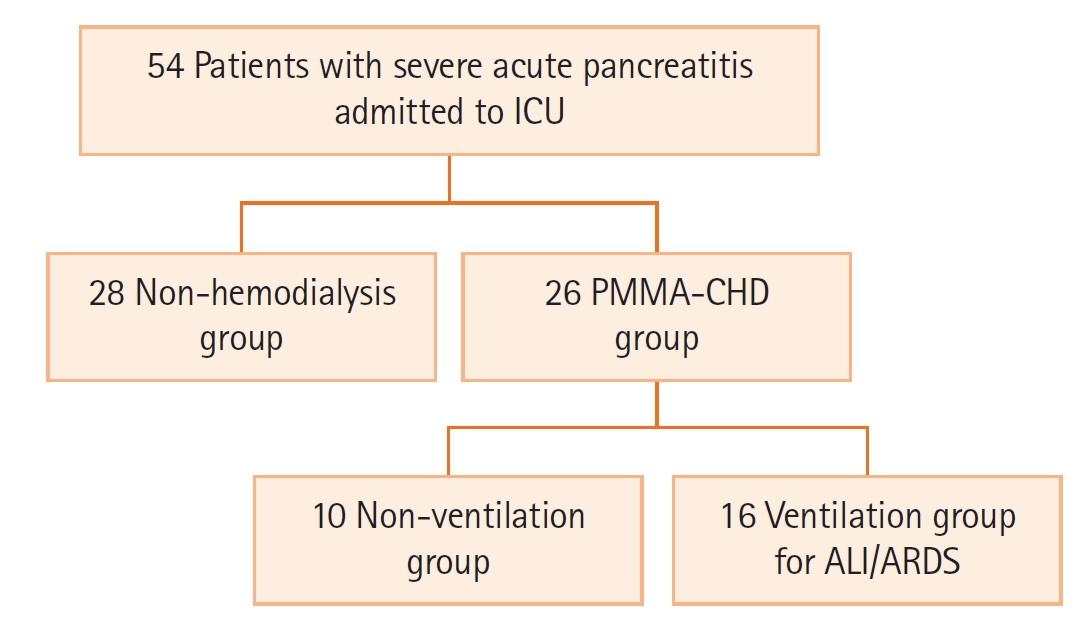
Flow diagram of patients with acute pancreatitis treated in the intensive care unit (ICU). A total of 54 patients with acute pancreatitis were admitted to our ICU. Among them, 26 patients required continuous hemodialysis with a polymethylmethacrylate membrane hemofilter (PMMA-CHD) during their ICU stay and 16 patients required ventilation for acute lung injury (ALI)/acute respiratory distress syndrome (ARDS).
Among 26 patients who required PMMA-CHD, 16 patients developed ALI/ARDS and consequently required mechanical ventilation with significant differences (Table 2). A total of 12 patients were intubated. Two patients required mechanical ventilation in the non-hemodialysis group (n=28). Patients in the ventilation group showed severe deteriorated lung and tissue involvement around the pancreas with significant high LIS and Balthazar CTSI (Table 2). The duration of hemodialysis therapy was significantly longer in the ventilation group than in the non-ventilation group; moreover, the length of ICU stay was longer in this group. However, there was no significant difference in the survival ratio between these two groups (Table 2).
Among the 16 ventilated patients, 7 showed further deterioration of their respiratory condition with sepsis (n=2), necrotizing pancreatitis (n=2), cardiac failure (n=2), or systemic infection with herpes simplex virus (n=1). High-flow-volume HDF was performed on these seven patients using a 2.1-m2 PMMA hemofilter intermittently between PMMA-CHD (Table 3). In these patients, the LIS was significantly increased with significantly longer periods for blood purification. However, these seven patients recovered fully and survived, as shown in Table 3.

Profile and data of seven critical cases requiring PMMA-CHD with additional intermittent HDF using a PMMA hemofilter
All the 26 patients in the PMMA-CHD group discontinued blood purification therapy after improvement in APACHE II score, SOFA score, KDIGO stage, and LIS (Figure 3). On day 28, all the 26 patients with PMMA-CHD survived, and 24 patients (92.3%) recovered fully and were discharged from the hospital (Table 1). In the non-hemodialysis group, 26 patients (92.9%) survived and were discharged from the hospital; however, two patients in this group died from severe alcoholic liver failure after recovering from SAP on days 26 and 29. In the PMMA-CHD group, two patients died; one patient in the non-ventilation group died of pancreatic cancer on day 59 and one patient in the ventilation group died of ICU-acquired weakness with severe pneumothorax from unidentified causes on day 58. No significant differences were noted in the final survival rate between the PMMA-CHD and non-hemodialysis groups and the ventilation and non-ventilation groups, as described above. Compared with the high estimated mortality ratio predicted using APACHE II score, the observed mortality in our study was obviously low, and the real mortality ratio did not increase in patients requiring blood purification (Table 1). Although the predicted mortality was significantly higher in the PMMA-CHD group than in the non-hemodialysis group, there were no significant differences in the observed mortality rate between these two groups (Table 1). The calculated standardized mortality ratio (SMR) was 0.76 in the non-hemodialysis group and 0.28 in the PMA-CHD group. Thus, the SMR was remarkably lower than the expected ratio, especially in the blood purification group of PMMA-CHD.
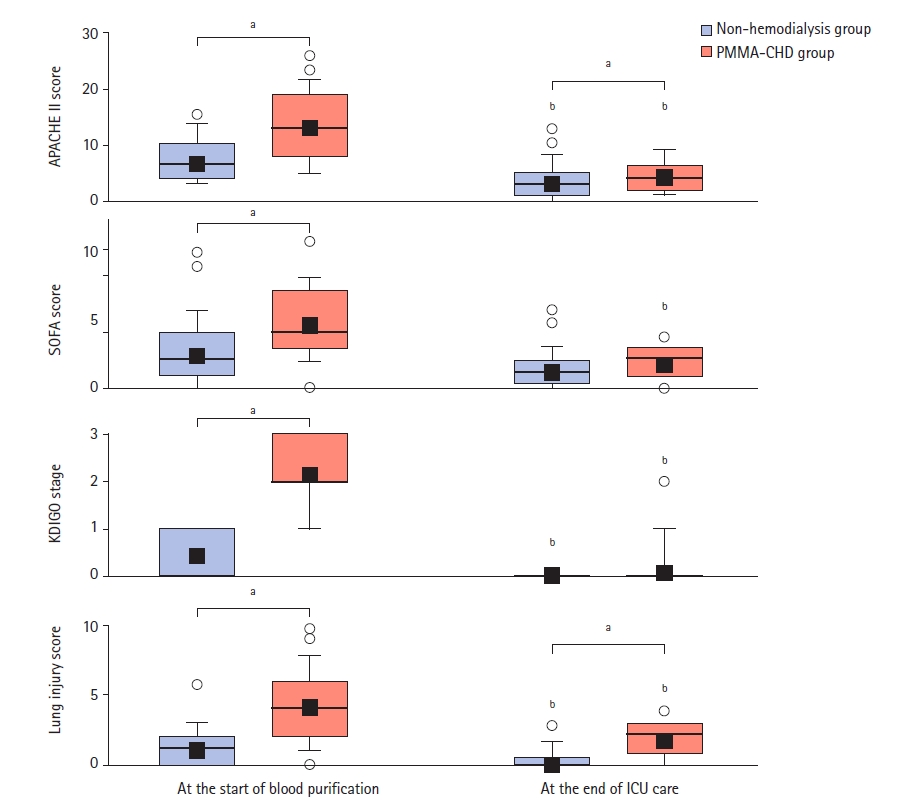
Changes of scores of Acute Physiology and Chronic Health Evaluation (APACHE) II score, Sequential Organ Failure Assessment (SOFA) score, Kidney Disease: Improving Global Outcome (KDIGO) stage, and lung injury score during intensive care unit (ICU) care. Blue boxes: non-hemodialysis group; red boxes: continuous hemodialysis with a polymethylmethacrylate membrane hemofilter (PMMA-CHD) group. Box, 25th–75th percentiles; Error bar, 10th and 90th percentiles; Bold horizontal line, median; closed square, mean value; Open circle, outlier. aP<0.05 as compared with values between the PMMA-CHD and non-hemodialysis groups; bP<0.05 as compared with values between values at the start and end of ICU care in each group.
DISCUSSION
Despite significant progress in the treatment and management, SAP remains a severe medical condition associated with MOF and poor clinical outcomes. SAP can often progress into AKI [3], wherein immune dysregulation, particularly overexpression of proinflammatory cytokines, is reportedly associated with organ failure [20]. Notably, the interleukin (IL)-6 and tumor necrosis factor (TNF)-α levels were shown to be associated with mortality in this disease [21]. Based on these findings, the use of blood purification therapies has been attempted to decrease the serum cytokine levels [22]. A PMMA hemofilter has been reported to reduce the cytokine levels in vivo and ex vivo [7,11].
It has been reported that continuous hemofiltration (CHF) ranging from 2,000 to 2,500 ml/hr using polysulfone filters reduced the TNF-α, IL-4, and IL-6 levels in patients with SAP complicated with pulmonary failure [22]. Moreover, PMMA hemofilters reportedly have a unique characteristic to adsorb proinflammatory cytokines, thereby yielding good clinical efficacy for patients with SAP [11]. Rasch et al. [23] reported that cytokine adsorption by an AN60 hemofilter was effective for stabilizing hemodynamics in SAP patients, with a decrease in the level of IL-6 or other inflammation markers. Comparing the 28-day survival rate in patients requiring continuous renal replacement therapy, acute blood purification therapy using an AN69 hemofilter showed better survival rates than that using a PMMA hemofilter [20]. Thus, blood purification therapy could be a useful option for the treatment of SAP patients. On the other hand, there was a report stating that the mortality of SAP was significantly higher in patients requiring blood purification therapy as compared to those without blood purification therapy [21]. Thus, blood purification therapy is still considered as a controversial procedure. However, in this study, SAP was improved by the use of PMMA-CHD (Figure 3). Intermittent PMMA-HDF during PMMA-CHD was used for seven patients whose condition deteriorated markedly due to sepsis or other systemic complications, and their complications were well managed. These different modes of blood purification possibly contribute to the management of complications, as discussed by Nishida et al. [14].
In patients with SAP who developed AKI, the mortality increases to between 20% and 80% [2,3]. In our study, the AKI in all the 26 patients with PMMA-CHD was successfully improved, and hemodialysis therapy was discontinued. ALI/ARDS in SAP also represents a substantial problem, with a reported mortality of up to 50% [6,24]. Gougol et al. [25] reported that the length of ICU stay was protracted in SAP patients with respiratory failure and that the mortality of SAP with MOF was 32.4%. In their analysis, patients with MOF were observed to mostly have respiratory failure. In our study, ALI/ARDS did not increase the mortality rates in patients in the hemodialysis group, even in patients who underwent ventilation, as shown in Tables 1 and 2.
A previous study has reported that systemic inflammation was associated with ICU-acquired weakness and indicated that IL-6, TNF-α, or other cytokines could play roles in this pathogenesis [26]. In our study, one patient with ICU-acquired weakness did not show any improvement during treatment with PMMA-CHD. Therefore, it remains unclear whether cytokine regulation with the PMMA hemofilter was effective for ICU-acquired weakness. The cost-effectiveness of blood purification therapy for SAP is another concern. Although the PMMA hemofilter was reported to adsorb the proinflammatory cytokines well, as described above, coagulation in hemofilters during blood purification due to chemostructural changes in membrane surface was found to be a complication [27]. Therefore, a high dose of the anticoagulant nafamostat mesilate was required [28]. Theoretically, CHF was considered to be effective for adsorbing cytokines [29], and it was reported that the use of CHF was significantly expensive compared with the use of CHD [30]. Based on these findings, we routinely use CHD instead of CHF and hemodiafiltration to maintain longer usage of the PMMA hemofilters in our medical practice. In contrast, we attempted to use additional intermittent PMMA-HDF for deteriorated patients with ARDS/ALI in this study. The combination of PMMA-CHD with intermittent PMMA-HDF showed effectiveness in most of such server patients, as shown in Table 3; however, the increased costs were noted. The indication of such a combination of blood purification therapies should be considered in future investigations.
This study has several limitations. First, the number of patients was small, and this was a single-center study, thereby limiting the generalization of the study findings. Second, hemofilters using other membrane types that do not absorb cytokines were not used as a control group; therefore, the efficacy of PMMA-CHD could not be clearly determined. Third, we did not measure the serum cytokine levels; therefore, we could not clearly demonstrate the relationship between the performance of cytokine adsorption and the improvement in organ failures. Fourth, considering the retrospective nature of this study, there is definitely a chance that we might have missed some relevant clinical information. Fifth, the problem of cost-effectiveness of blood purification using a PMMA hemofilter was still controversial. These points should be addressed in further studies.
Key Message
▪ Blood purification using polymethylmethacrylate (PMMA) hemofilters could be a potential treatment method for severe acute pancreatitis (SAP), given that PMMA hemofilters could adsorb proinflammatory cytokines.
▪ Continuous hemodialysis using a PMMA hemofilter could improve acute kidney injury (AKI) and pulmonary failure in SAP patients.
▪ Additional intermittent PMMA hemodiafiltration was thought to be effective in patients developing severe lung injury.
▪ Although blood purification therapy is not a standard therapy for SAP patients, it was suspected that the blood purification using a PMMA hemofilter is effective for the treatment of AKI and pulmonary failure in SAP patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: all authors. Data curation: all authors. Formal analysis: KK. Methodology: KK, YS, KI. Project administration: RN. Visualization: SY. Writing–original draft: KK. Writing–review & editing: KK.