Prevalence and clinical impact of vitamin D deficiency in critically ill Korean patients with traumatic injuries: a single-center, prospective, observational study
Article information
Abstract
Background
This study investigated the prevalence and impact of 25-hydroxyvitamin D (25(OH) vitamin D) deficiency in critically ill Korean patients with traumatic injuries.
Methods
This prospective observational cohort study assessed the 25(OH) vitamin D status of consecutive trauma patients admitted to the trauma intensive care unit (TICU) of Kyungpook National University Hospital between January and December 2018. We analyzed the prevalence of 25(OH) vitamin D deficiency and its impact on clinical outcomes.
Results
There were no significant differences in the duration of mechanical ventilation (MV), lengths of TICU and hospital stays, and rates of nosocomial infection and mortality between patients with 25(OH) vitamin D <20 ng/ml and those with 25(OH) vitamin D ≥20 ng/ml within 24 hours of TICU admission. The duration of MV and lengths of TICU and hospital stays were shorter and the rate of nosocomial infection was lower in patients with 25(OH) vitamin D level ≥20 ng/ml on day 7 of hospitalization. The duration of MV, lengths of TICU and hospital stays, and nosocomial infection rate were significantly lower in patients with increased concentrations compared with those with decreased concentrations on day 7 of hospitalization, but the mortality rate did not differ significantly.
Conclusions
The 25(OH) vitamin D level measured within 24 hours after TICU admission was unrelated to clinical outcomes in critically ill patients with traumatic injuries. However, patients with increased 25(OH) vitamin D level after 7 days of hospitalization had better clinical outcomes than those with decreased levels.
INTRODUCTION
Vitamin D is an important pro-hormone that is produced in the skin after exposure to ultraviolet (UV) B radiation or is obtained from the diet [1-4]. It is hydroxylated in the liver to 25-hydroxyvitamin D (25(OH) vitamin D) and further hydroxylated in the kidney to 1,25-dihydroxyvitamin D (1,25(OH)2 vitamin D), the active hormone involved in serum calcium and phosphorus homeostasis for optimal neuromuscular function. Vitamin D plays an important role in the innate and acquired immune systems, especially in patients with infectious disease, diabetes mellitus, myocardial infarction, cardiac failure, stroke, Alzheimer disease, osteoporosis, inflammatory bowel disease, chronic obstructive airway disease, and autoimmune disease [5-7]. In particular, vitamin D deficiency is identified frequently in patients in the intensive care unit (ICU); patients in the ICU have lower vitamin D level than the general population. Vitamin D level in critically ill patients can affect their clinical outcomes, such as the duration of mechanical ventilation (MV) and rates of complications, morbidity, and mortality [5-10]. Trauma patients often are hospitalized for sudden accidents that occur during daily activities. Therefore, deficiency of vitamin D, which is synthesized by exposure to UV light, is less prevalent in these patients than in those hospitalized with diseases. In addition, trauma leads to a very serious stress response, including inactivation of the immune system, leaving trauma patients vulnerable to infections such as bacteremia, urinary tract infection, pneumonia, and wound infections, as well as complications during hospitalization. To date, only a few studies have assessed the effects of blood vitamin D level on clinical outcomes in trauma patients. Therefore, the present study investigated the prevalence of vitamin D deficiency in patients with severe trauma and the relationship between serum 25(OH) vitamin D level and clinical outcomes of duration of MV, lengths of trauma ICU (TICU) and hospital stays, and rates of nosocomial infection and mortality.
MATERIALS AND METHODS
This prospective observational cohort study included all trauma patients aged ≥ 18 years who were consecutively admitted to the TICU at the trauma center of Kyungpook National University Hospital within 24 hours of trauma injury between January and December 2018. The study protocol was in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Kyungpook National University Hospital (IRB No. 2016-11-025-002). Written informed consent was obtained from all patients or their family members. Patients who did not stay in the TICU for ≥ 24 hours or who were administered multivitamin supplements or medications that could affect 25(OH) vitamin D level within 7 days of administration were excluded. The following patient information was collected from the electronic medical record system of the hospital: age, sex, body mass index (BMI), trauma mechanism, nutrition status (enteral or parenteral nutrition for ≥ 3 days before the test on day 7), presence of shock (systolic blood pressure < 90 mm Hg or heart rate > 120/min) on admission, operation within 7 days, and measures of severity such as the Glasgow coma scale (GCS) score, injury severity score (ISS), Acute Physiology and Chronic Health Evaluation (APACHE) II score, Sequential Organ Failure Assessment (SOFA) score, and Simplified Acute Physiology Score III (SAPS III). Clinical outcomes were the duration of MV, lengths of TICU and hospital stays, and rates of nosocomial infection and mortality. Blood 25(OH) vitamin D level was measured within 24 hours and after 7 days of TICU admission using the reference standard of liquid chromatography and tandem mass spectrometry (Quest Diagnostics Lab, Valencia, CA, USA). Based on a previously published study on vitamin D level in critically ill patients [9], the patients were classified into two groups according to blood 25(OH) vitamin D level measured within 24 hours of TICU admission: group A ( < 20 ng/ml [50 nmol/L]) and group B ( ≥ 20 ng/ml [50 nmol/L]). Continuous variables were reported as mean ± standard deviation and compared using Student t-test, whereas categorical variables were reported as proportions (percentages) and were compared using Pearson’s chi-square test or Fisher’s exact test, as appropriate. The association between parameters recorded in our database was tested using binary logistic regression analysis. Factors associated with the outcome were used to build multivariate forward stepwise logistic regression models and determine independent factors related to vitamin D level and nosocomial infection rate. All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), with P-values less than 0.05 considered statistically significant.
RESULTS
Patient Demographics
This study included 191 consecutive patients admitted to the TICU who met our inclusion criteria. Of these patients, 145 (75.9%) were men, and 46 (24.1%) were women; the mean age was 53.1 ± 20.6 years. Most patients (182/191, 95.3%) were hospitalized after blunt trauma injury. These patients had a mean GCS score of 12.3 ± 4.0 (range, 3–15), an ISS of 17.4 ± 9.0 (range, 1–75), APACHE II score of 10.7 ± 7.3, SOFA score of 3.3 ± 3.1, and SAPS III of 45.2 ± 15.7.
Distribution and Seasonal Variation in 25(OH) Vitamin D Level at TICU Admission
The mean serum 25(OH) vitamin D level within 24 hours of TICU admission was 10.6 ± 7.0 ng/ml. Of the 191 patients, 109 (57.1%) had 25(OH) vitamin D deficiency ( < 10 ng/ml), 78 (40.8%) had 25(OH) vitamin D insufficiency (10–29 ng/ml), and four (2.1%) had 25(OH) vitamin D sufficiency (30–100 ng/ml) (Table 1). To determine whether there were seasonal variations in serum 25(OH) vitamin D level, the levels in the study patients were compared to those of 130 other patients that were admitted to the TICU from April to September and to the levels of 61 patients admitted to the TICU from October to March. The mean 25(OH) vitamin D levels in these two groups were 10.4±7.2 and 10.9±6.6 ng/ml, respectively, showing no seasonal variations (P = 0.638).
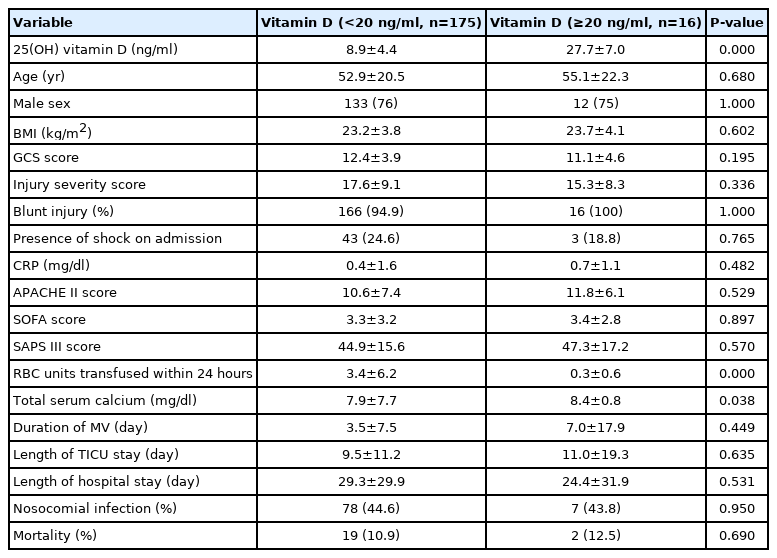
Comparison of Initial 25(OH) Vitamin D Level on Day 1
There were no statistical differences in age, sex, BMI, GCS score, ISS, injury mechanism, presence of shock, APACHE II score, SOFA score, and SAPS III between patients with 25(OH) vitamin D level < 20 ng/ml and those with 25(OH) vitamin D level ≥ 20 ng/ml. In contrast, the amount of red blood cells (RBCs) transfused within 24 hours of admission was significantly higher and the serum total calcium was significantly lower in patients with 25(OH) vitamin D level < 20 ng/ml than in those with 25(OH) vitamin D level ≥ 20 ng/ml. However, there were no statistically significant differences between the groups in terms of the duration of MV, lengths of TICU and hospital stays, and rates of nosocomial infection and mortality (Table 2).
Comparison of 25(OH) Vitamin D Level on Day 7
Serum 25(OH) vitamin D level was measured in 153 (80.1%) of 191 patients 7 days after TICU admission. The mean 25(OH) vitamin D level in these patients was 9.4 ± 7.5 ng/ml. The GCS score, SOFA score, duration of MV, lengths of TICU and hospital stays, and rate of nosocomial infection differed significantly between patients with 25(OH) vitamin D level < 20 ng/ml and those with 25(OH) vitamin D level ≥ 20 ng/ml on day 7. However, there were no statistically significant differences between these two groups in terms of age, sex, BMI, ISS, SAPS III, units of RBCs transfused, presence of shock, status of nutrition, and rate of mortality (Table 3).
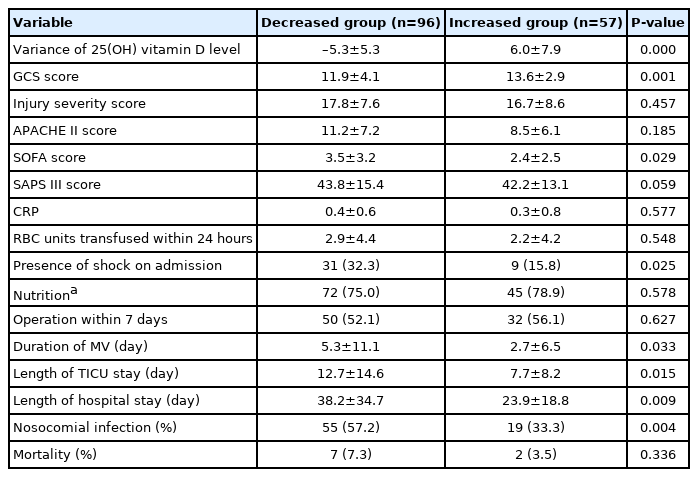
Clinical Outcomes of TICU Patients That Showed Increased and Decreased 25(OH) Vitamin D Level from Day 1 to Day 7 of Hospitalization
Of the 153 patients, 57 (37.3%) showed an increase and 96 patients (62.7%) showed a decrease in 25(OH) vitamin D level from day 1 to day 7. The duration of MV, lengths of TICU and hospital stays, and nosocomial infection rate were significantly lower in patients in whom the level increased than in those in whom the level decreased, although there was no betweengroup difference for nutrition status and rate of mortality (Table 4).
Logistic Regression Analysis for Risk Factors Associated with Nosocomial Infection
Risk factors associated with nosocomial infection indicated that APACHE II score, presence of shock on admission, and length of hospital stay were independent factors, based on multivariate analysis (Table 5).
DISCUSSION
Vitamin D deficiency is a common problem in the general population [8-10]. The 2008 Korean National Health and Nutrition Examination Survey found that the prevalence of vitamin D insufficiency (25(OH) vitamin D level; 10–30 ng/ml) was 82.6% and that of deficiency (25(OH) vitamin D <10 ng/ml) was 7.9% in the general Korean population [1]. Vitamin D deficiency is the most common nutritional deficiency in the United States [8]. The causes of vitamin D deficiency in the general population are multifactorial, including low vitamin D content in foods, blocking of vitamin D synthesis in the skin by the use of sunscreen, and reduced vitamin D synthesis in aging skin. In obesity, vitamin D is stored in fat cells instead of the liver. Chronic renal disease, liver failure, seasonal variations in exposure to sunlight in spring and winter, living in an urban area, and working indoors also are factors associated with vitamin D deficiency. The half-life of 25(OH) vitamin D is 15 days; hence, because trauma patients are often hospitalized after accidents in routine daily living, the initial vitamin D level in trauma patients is likely to be similar to that in the general population. Measurement of vitamin D level in trauma patients within 24 hours of TICU admission showed that almost all patients (97.9%) had 25(OH) vitamin deficiency ( < 10 ng/ml) or insufficiency (10–29 ng/ml). Similarly, a study on critically ill patients with traumatic injuries in the United States found that 96.2% had deficient or insufficient level of vitamin D [11]. However, these values were higher than in the general population mentioned above. Since vitamin D measurements for trauma patients were conducted after admission to the TICU and not immediately after arrival, fluid resuscitation in the emergency room, decreased serum calcium level due to RBC transfusion, and acute inflammatory conditions might have affected these differences.
In a study of traumatic patients in the United States, penetrating injuries, African-American race, and obesity were significant risk factors for vitamin D deficiency. In contrast, the severity of injury, extent of inflammation (elevated C-reactive protein level), and hospital admission in winter did not significantly influence the prevalence of vitamin D deficiency [11]. The results of our study were similar, but penetrating injuries did not affect our results. The initial level of bleeding was not large in the Korean cohort because the most common penetrating injuries in South Korea are stab injuries with a moderate degree of damage, in contrast to the majority of gun-shot penetrating injuries in the United States that are associated with a severe degree of damage. This is supported by the amount of RBCs transfused within 24 hours, and the corresponding decrease in total calcium level, which affected the vitamin D level in our study.
Although several studies have evaluated the relationship between vitamin D deficiency and clinical outcomes in critically ill patients, the associations between vitamin D level and clinical outcomes, such as the duration of MV, lengths of ICU and hospital stays, and mortality are unclear [5-19]. For example, in a previous study, the length of ICU stay, surgical ICU costs, and mortality were significantly associated with vitamin D deficiency [8]. Another previous study reported that serum 25(OH) vitamin D level within 24 hours of ICU admission was associated with prolonged hospitalization, readmission, and mortality, suggesting the need for randomized trials to determine whether vitamin D supplementation can improve these clinically relevant outcomes in surgical ICU patients [9]. A meta-analysis found that 25(OH) vitamin D level < 50 nmol/L (< 20 ng/ml) was associated with high rates of infection, sepsis, 30-day mortality, and in-hospital mortality, suggesting that vitamin D deficiency increases the susceptibility of critically ill patients to severe infection and death [10]. In a previous study, patients with vitamin D deficiency or insufficiency had higher rates of complications and longer ICU and hospital stays than patients with normal vitamin D level [12]. Further, vitamin D deficiency had a significant impact on the length of stay, organ dysfunction, and the rate of infection [15]. Plasma 25(OH) vitamin D level measured on ICU admission was inversely associated with the duration of respiratory support [16]. Moreover, vitamin D status could be a modifiable risk factor for non-home discharge in surgical ICU patients [17], and vitamin D deficiency in patients with traumatic brain injury is associated with impaired cognitive function and severe depressive symptoms [18]. However, one study reported that although vitamin D insufficiency was associated with severe illness, vitamin D level was not significantly associated with the length of ICU stay or patient mortality [19]. Our study also found no significant differences between serum 25(OH) vitamin D level measured within 24 hours of TICU admission and clinical outcomes. Both the amount of RBCs transfused within 24 hours and the total calcium level were high in the group with low 25(OH) vitamin D level ( < 20 ng/ml) within 24 hours of TICU admission. A hypothesis for this is that serum dilution by massive resuscitation in the early stage and calcium reduction due to many RBC transfusions impact vitamin D level. In contrast, the duration of MV, lengths of TICU and hospital stays, and rate of nosocomial infection were significantly lower in patients with 25(OH) vitamin D ≥ 20 ng/ml than in those with 25(OH) vitamin D < 20 ng/ml on day 7 of admission. Moreover, the duration of MV, lengths of TICU and hospital stays, and rate of nosocomial infection were significantly lower in patients in whom the 25(OH) vitamin D level increased from day 1 to day 7 than in patients in whom the level did not increase. On multivariate analysis, only APACHE II scores and the length of hospital stay were independent variables that affected the rate of nosocomial infection. Based on the above results, at first glance, the effects of vitamin D appear to be an important risk factor for clinical outcomes. However, it is unclear whether the clinical outcome was poor due to low vitamin D level or whether the presence of multiple complications and inflammation in severe trauma patients with poor clinical outcomes affected vitamin D level.
This study has several limitations. First, factors such as intake of vitamin D and drugs that affect vitamin metabolism before hospitalization, and the general environment of the patients, such as occupation, was not analyzed. Second, the heterogeneity of the trauma experienced by these patients and other variables could affect clinical outcomes. Third, the small sample size produced inevitable selection bias. Therefore, future studies with larger cohorts are required to corroborate these results. Although this study did not find a clear effect of vitamin D level on clinical outcomes in trauma patients, to our knowledge, this is the first study to examine vitamin D level in trauma patients in South Korea, and the study findings can be used as a basis for future investigations.
KEY MESSAGES
▪ The majority of patients with traumatic injuries were either 25-hydroxyvitamin D (25(OH) vitamin D) deficient or insufficient.
▪ The 25(OH) vitamin D level measured within 24 hours after trauma intensive care unit admission was unrelated to clinical outcomes in critically ill patients with traumatic injuries.
▪ Patients with increased 25(OH) vitamin D level after 7 days of hospitalization had better clinical outcomes than those with decreased D level.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: JP, KHL. Data curation, Formal analysis, & Methodology: all authors. Funding acquisition: JJ. Project administration & Visualization: all authors. Writing–original draft: JP. Writing–review & editing: KHL.
Acknowledgements
This work was supported by a grant by the Biomedical Research Institute, Kyungpook National University Hospital (2018).