Clinical implications of pleural effusion following left ventricular assist device implantation
Article information
Abstract
Background
Studies on the association between pleural effusion (PE) and left ventricular assist devices (LVADs) are limited. This study aimed to examine the characteristics and the clinical impact of PE following LVAD implantation.
Methods
This study is a prospective analysis of patients who underwent LVAD implantation from June 2015 to December 2022. We investigated the prognostic impact of therapeutic drainage (TD) on clinical outcomes. We also compared the characteristics and clinical outcomes between early and late PE and examined the factors related to the development of late PE.
Results
A total of 71 patients was analyzed. The TD group (n=45) had a longer ward stay (days; median [interquartile range]: 31.0 [23.0–46.0] vs. 21.0 [16.0–34.0], P=0.006) and total hospital stay (47.0 [36.0–82.0] vs. 31.0 [22.0–48.0], P=0.002) compared to the no TD group (n=26). Early PE was mostly exudate, left-sided, and neutrophil-dominant even though predominance of lymphocytes was the most common finding in late PE. Patients with late PE had a higher rate of reintubation within 14 days (31.8% vs. 4.1%, P=0.004) and longer hospital stays than those without late PE (67.0 [43.0–104.0] vs. 36.0 [28.0–48.0], P<0.001). Subgroup analysis indicated that female sex, low body mass index, cardiac resynchronization therapy, and hypoalbuminemia were associated with late PE.
Conclusions
Compared to patients not undergoing TD, those undergoing TD had a longer hospital stay but not a higher 90-day mortality. Patients with late PE had poor clinical outcomes. Therefore, the correction of risk factors, like hypoalbuminemia, may be required.
INTRODUCTION
Left ventricular assist device (LVAD) implantation is an important treatment method for prolonging lives and improving the quality of life in patients with advanced heart failure [1]. Pleural effusion (PE) is common after cardiac surgery, including coronary artery bypass grafting (CABG), valve replacement, heart transplantation, and LVAD implantation [2-5]. Patients who develop PE may develop a poor prognosis after cardiac surgery. While PE drainage aids in the characterization and diagnosis of PE, it remains controversial with concern to its clinical benefits after cardiac surgery [6-9]. Additionally, it is known that early PE, occurring within 30 days after surgery, and late PE, appearing more than 30 days after surgery, have different causes and characteristics [10-15]. Studies focusing on PE related to LVAD implementation are limited, and none have examined the clinical impact of PE after LVAD implantation [10,16,17]. Therefore, the aims of this study were to analyze clinical outcomes by comparing patients who underwent therapeutic drainage (TD) after LVAD implantation and those who did not and investigate the differences between early and late PE. Additionally, we conducted subgroup analyses to assess the clinical outcomes and predictors in patients with late PE.
MATERIALS AND METHODS
Study Design
This prospective study analyzed all patients who underwent LVAD implantation at a single, high-volume hospital center between June 2015 and December 2022. Until 2021, the HeartWare ventricular assist device (HVAD; Medtronic) was LVAD type, which then transitioned to the HeartMate 3 (HM3; Abbott Laboratories) starting in 2022. We separated patients into two groups: those who received TD (TD group) and those who did not (no TD group). Depending upon the clinical judgment of the physicians after evaluating the quantity of PE through serial chest radiographs or bedside lung ultrasound, TDs were initiated. This study received approval from the Institutional Review Board of Asan Medical Center (No. 2018-0234), and all participants provided written informed consent.
Pleural Effusion and Therapeutic Drainage
The amount of PE was categorized as small (less than 1/3 of the hemithorax and presenting costophrenic angle blunting on chest radiography), moderate (between 1/3 and 2/3 of the hemithorax), or large (more than 2/3 of the hemithorax). All the large PE cases underwent TD, while moderate PEs only had TD based on the clinical situation, particularly for relief of dyspnea. In some cases, small PEs were subject to TD for effusion analysis, especially when diagnostic uncertainty persisted. TDs were performed through insertion of percutaneous catheter drainage (PCD). Experienced clinicians performed PCD insertion using 7-Fr or 8-Fr catheters with bedside echocardiography or fluoroscopy using the Seldinger technique. This was performed to reduce the risk of recurrent procedures and bleeding while considering postoperative anticoagulation. Light’s criteria were used to classify PEs obtained through TD as exudate [18].
Outcomes
The primary outcome was 90-day mortality following LVAD implantation. Secondary outcomes were reintubation rate within 2 weeks after surgery, duration of ventilator support, and length of intensive care unit (ICU) or hospital stay postoperatively.
Subgroup Analysis
Subsequently, patients were divided into early PE and late PE groups. Early PE was defined as occurring within 30 days postoperatively. Conversely, late PE was defined as residual PE that persisted for more than 30 days postoperatively. For PEs, the decision to insert PCDs was based on the clinician’s judgment, and subsequent PE analysis was performed. Furthermore, we compared clinical outcomes between the two groups. Additionally, we aimed to identify potential risk factors associated with the development of late PEs.
Statistical Analysis
Continuous variables were presented depending on their distribution. When continuous variables were normally distributed, they were expressed as the mean and standard deviation and were analyzed using Student t-test. Conversely, continuous variables that did not follow a normal distribution were expressed as the median and interquartile range and analyzed using the Mann-Whitney rank-sum test. Categorical variable data were presented as numbers with percentages and analyzed using Fisher’s exact test or a chi-square test. P-value <0.05 was considered statistically significant. To identify predictors of late PEs, univariate analysis was performed, followed by stepwise multivariate logistic regression using variables with P-values <0.1 or clinical significance factors from the univariate analysis. Kaplan-Meier analysis and the log-rank test were used to compare 90-day survival rates between the TD and no TD groups. Statistical analyses were performed using R program version 4.2.3 (R Foundation for Statistical Computing).
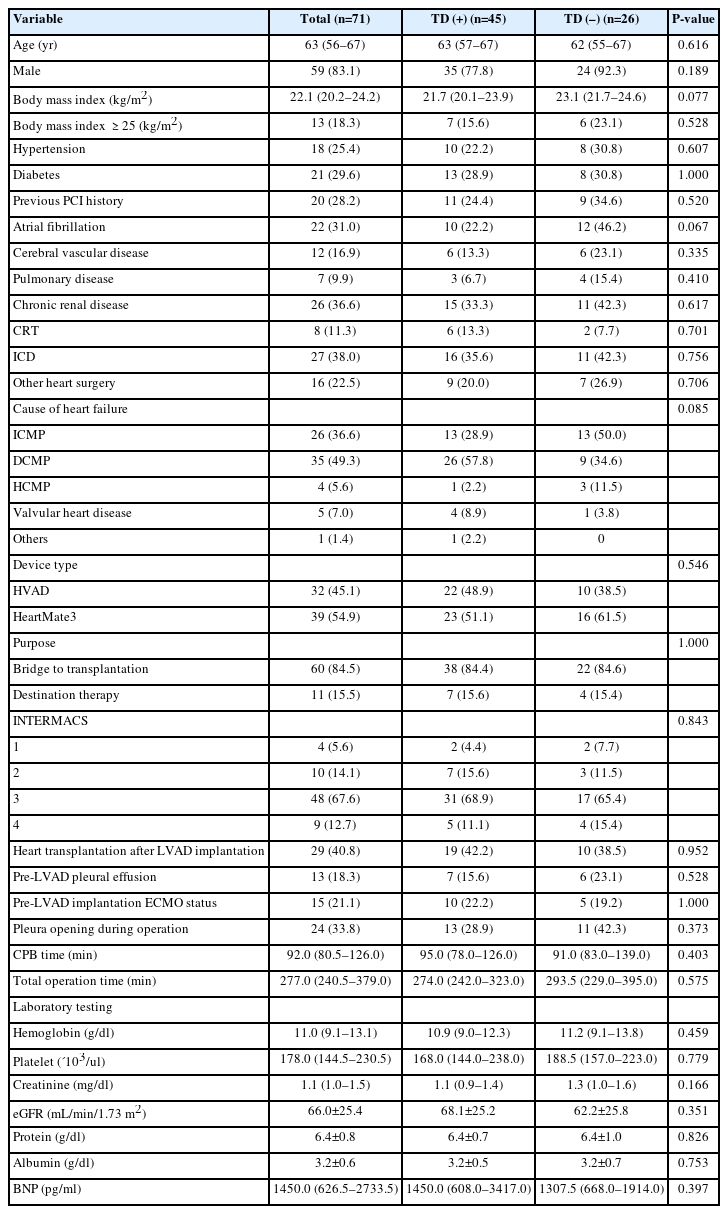
RESULTS
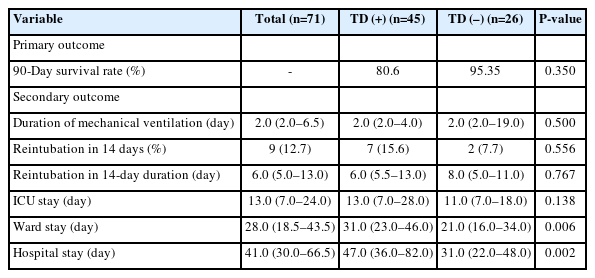
A total of 71 patients underwent LVAD implantation from June 2015 to December 2022. Among them, 45 patients underwent TD (TD group), while 26 did not (no TD group). All first postsurgical TDs were performed within 30 days. The baseline characteristics of both groups are shown in Table 1. The mean age of the patients was 63.0 years. In the TD and no TD groups, 77.8% and 92.3% of participants were male, respectively. The percentage of patients with a body mass index (BMI) exceeding 25 kg/m2 was 15.6% (TD group) and 23.4% (no TD group). Hypertension was reported in 22.2% (TD group) and 38.5% (no TD group) of patients, and 28.9% (TD group) and 30.8% (no TD group) of patients had diabetes. History of percutaneous coronary intervention was present in 24.4% (TD group) and 34.6% (no TD group). The prevalence of atrial fibrillation was 22.2% (TD group) and 46.2% (no TD group). Cerebral vascular disease was present in 13.3% (TD group) and 23.1% (no TD group) of patients. The percentage of patients with pulmonary disease was 6.7% (TD group) and 15.4% (no TD group). Furthermore, 33.3% and 42.3% of patients in the TD and the no TD group had chronic renal disease, respectively. However, none of these differences were statistically significant. The most common etiology was dilated cardiomyopathy in the TD group (57.8%) and ischemic cardiomyopathy in the no TD group (50.0%). Regarding the type of device, the HVAD was more frequently used in the TD group (48.9%), while HM3 had a higher usage rate in the no TD group (61.5%). No significant difference was observed in the two groups concerning the purpose for LVAD implantation or the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) profile. The rate of postsurgical heart transplantation was similar in the two groups (42.2% vs. 38.5% for TD group vs. no TD group, P=0.952), and the history of extracorporeal membrane oxygenation before surgery between groups was not significantly different (22.2% vs. 19.2%, P=1.000). Factors related to the surgical procedure, such as whether the pleura was opened during the operation, cardiopulmonary bypass (CPB) time, and total operative time, did not significantly differ between groups. Additionally, all preoperative laboratory data were similar in the groups. The clinical outcomes of TD following LVAD implantation are shown in Table 2. The 90-day survival rate was not significantly different between groups (80.6% vs. 95.4%, P=0.350). The duration of mechanical ventilation was also similar in the two groups (2.0 days [2.0–4.0] vs. 2.0 days [2.0–19.0], P=0.500) and the rates of reintubation within 14 days were comparable (15.6% vs. 7.7%, P=0.556). The length of ICU stay was similar between groups (13.0 days [7.0–28.0] vs. 11.0 days [7.0–18.0], P=0.138). However, compared to the no TD group, the TD group had a longer ward stay (31.0 days [23.0–46.0] vs. 21.0 days [16.0–34.0], P=0.006) and total hospital stay following LVAD implantation (47.0 days [36.0–82.0] vs. 31.0 days [22.0–48.0], P=0.002). The Kaplan-Meier curve (Figure 1) shows the 90-day survival probability in the two groups, with no significant difference (hazard ratio, 0.73; 95% confidence interval [CI], 0.25–2.12; log-rank P=0.542).
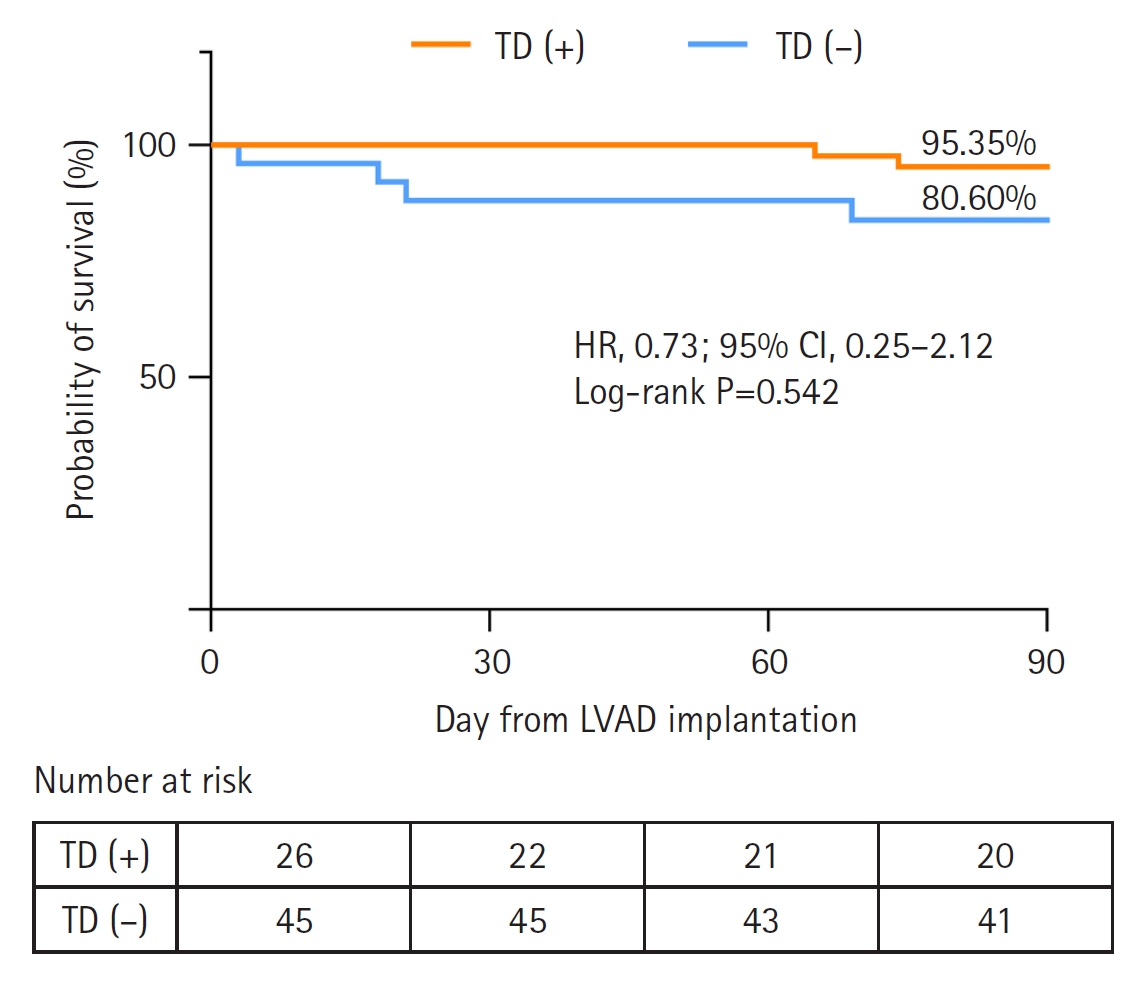
Ninety-day survival curves for patients with and without therapeutic drainage (TD). HR: hazard ratio; CI: confidence interval; LVAD: left ventricle assist device.
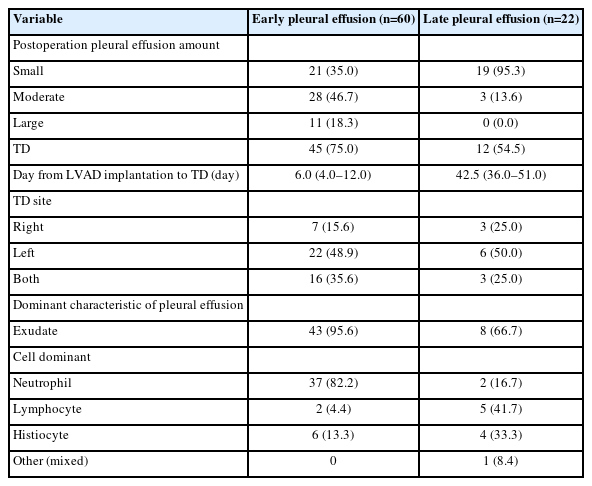
Additionally, we compared the characteristics of early and late PE. The features of early and late PE are shown in Table 3. Among the 60 patients with early PE, 45 (75%) underwent TD; among the 22 with late PE, this rate was 54.5%. The median time from surgery to TD was 6.0 days (4.0–12.0) and 42.5 days (36.0–51.0) for early and late PE patients, respectively. In the late PE cases, the duration from LVAD implantation to TD represented additional PCD insertion at 30 or more days following surgery. All patients in the late PE group had early PEs within 30 days following LVAD implantation. Among these, 20 patients in the late PE group received TD within 30-day postoperation; subsequently, these individuals encountered recurring or residual PEs beyond the initial 30 days following LVAD implantation. Importantly, the late PE group did not exhibit cases of large PE; instead, only small or moderate amounts of PE were observed. Among the patients with early PE, 65.0% had a moderate or large amount, whereas 95.3% of late PE cases had a small amount. Both early and late PE groups predominantly received TD on the left side (48.9% vs. 50.0%), and exudate was dominant in both groups (95.6% vs. 66.7%). In the early PE group, 82.2% had a neutrophil-dominant exudate composition. In the late PE group, 41.7% of patients had lymphocyte-dominant exudate composition, and 33.3% of patients had histiocyte-dominant exudate composition.
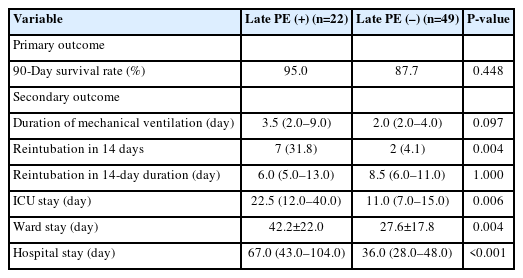
When comparing clinical outcomes based on the presence or absence of late PE (Table 4), the 90-day mortality rate between the two groups was not significantly different (95.0% vs. 87.7%, P=0.448). The duration of mechanical ventilation and the duration of reintubation within 14 days after surgery did not differ significantly between the two groups (3.5 days [2.0–9.0] vs. 2.0 days [2.0–4.0], P=0.09 and 6.0 days [5.0–13.0] vs. 8.5 days [6.0–11.0], P=1.000, respectively). Patients with late PE had a higher frequency of reintubation within 14 days (31.8% vs. 4.1%, P=0.004) and prolonged ICU stay (22.5 days [12.0–40.0] vs. 11.0 days [7.0–15.0], P=0.006) than those without late PE. Late PE groups had both significantly longer ward stay (42.2±22.0 days vs. 27.6±17.8 days, P=0.004) and hospital stay (67.0 days [43.0–104.0] vs. 36.0 days [28.0–48.0], P<0.001).
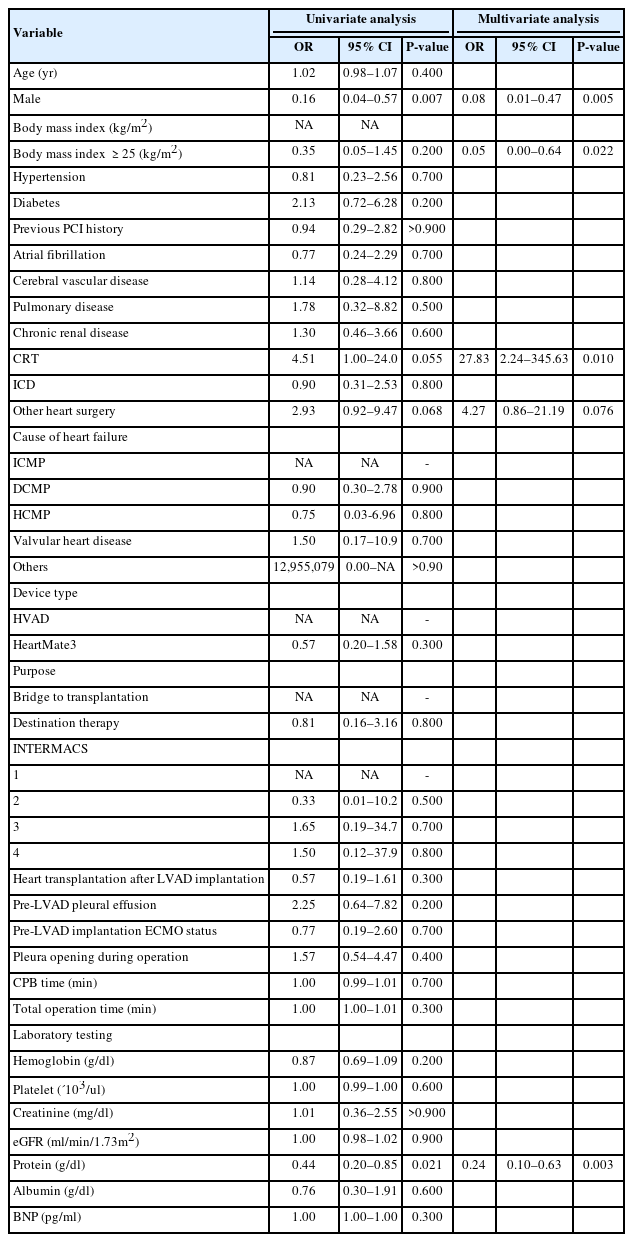
When identifying risk factors related to late PE (Table 5), cardiac resynchronization therapy (CRT) and lower protein levels were associated with the occurrence of late PEs (odds ratio [OR], 27.83; 95% CI, 2.24–345.63; P=0.010 and OR, 0.24; 95% CI, 0.10–0.63; P=0.003, respectively). Male sex (OR, 0.05; 95% CI, 0.00–0.64; P=0.022) and BMI exceeding 25 kg/m2 (OR, 0.08; 95% CI, 0.01–0.47; P= 0.005) decreased the risk of late PE occurrence.
DISCUSSION
This study compared patients with PE according to its onset and whether they underwent TD. First, the association of PE with TD after LVAD implantation and with mortality at 90 days or the duration of intubation was not significant. However, the total hospitalization period and general ward stay were significantly longer in the TD group compared to the no TD group. Second, early and late PE showed different characteristics. The rate of reintubation within 14 days for patients with late PE was higher than that of patients without late PE. Compared to patients without late PE, those with late PE had a significantly longer overall hospitalization time. Female sex, low BMI, and low protein levels were predictors of late PE occurrence. Our study provides valuable insights as the first to examine clinical outcomes associated with TD after LVAD implantation and the differences between early and late PE.
Compared to patients without PE, those who developed PE after cardiac surgery and needed secondary drainage had a significantly longer hospital stay and a higher mortality rate. PE has been associated with worse outcomes after cardiac surgery [7]. In a single-center cohort study, TD after LVAD implantation was related to prolonged length of stay [17]. A large multi-center observational study reported that critically ill patients with PE had increased mortality, and those who required TD had worse outcomes [8]. The total hospitalization period and general ward stay of the TD group were significantly longer compared to those of the no TD group. The 90-day survival rate did not differ significantly between the two groups (95.35% vs. 80.60%, P=0.350). Similarly, the duration of mechanical intubation did not differ significantly between the TD group and the no TD group (6.0 days [5.5–13.0] vs. 8.0 days [5.0–11.0], P=0.767). The lack of statistical significance may be attributed to the small sample size. Previous studies have shown that the duration of mechanical intubation is significantly longer in patients with PE after cardiac surgery, suggesting that TD might help reduce the duration of mechanical intubation [7]. Patients experienced a decrease in symptoms and increased walking distance 1 month postoperatively when TD was performed [19].
Early PE, defined as appearing within 30 days after cardiac operation, is typically small, neutrophil-dominant, and left-sided [11]. After cardiac surgery, early PE is common, occurring in 40%–80% of patients [4]. The causes of this are factors such as pleural damage during surgery; topical cooling; an early sign of postcardiac injury syndrome; and surgical disruption of the mediastinal lymphatic channels [12-14]. Our findings showed that the incidence of pleural opening between the two groups was not significantly different. Considering the similarities in the characteristics of early PE in CABGs and LVAD implantation, pleura- and pericardium-related surgical injuries may be the main cause of PE in patients undergoing LVAD. The absence of bacteria in PE and the dominance of neutrophils suggest that early PE may be primarily attributed to surgically related inflammation rather than infection. Furthermore, in late PEs, lymphocyte-dominant composition was the most common (41.7%) and late PEs were small in amount (95.3%). This is consistent with previous findings on PE after LVAD implantation [10]. Late PEs are generally small, and only 10% of late PEs correspond to a large amount in patients undergoing CABG [15]. Guha et al. [10] demonstrated that all late PEs were lymphocyte-dominant, and these findings suggested that inflammation may be the main reason for late PE in patients undergoing LVAD. Prolonged CPB time has been found to increase the incidence of PE [20,21]. Our findings showed that CPB time was not associated with PE in either the TD or no TD group. Histiocytic pleural effusion (HisPE) is defined as a PE in which histocytes account for more than 50% of all white blood cells [22]. In this study, four of six (66%) cases of early PE and all four (100%) cases of late PE met the classification of HisPE. An association between HisPE and malignancy has been reported; this is because histiocytes are tissue macrophages that tend to proliferate under increased reactive conditions caused by malignancy or inflammation. The cytology and culture for the PEs in this study were all negative, suggesting increased pleural inflammatory conditions as the cause of HisPEs.
In the subgroup analysis, factors of female and lower BMI were associated with a higher occurrence of late PE. Labidi et al. [4] found that female sex was associated with PE after cardiac surgery, although the reasons for the association remain unclear but could be attributed to smaller vascular volume. Furthermore, they reported that predictors of PE, including peripheral vascular disease, longer surgery time, and use of antiarrhythmic agents, may be associated with left ventricular dysfunction [4]. We identified CRT as a potential cause of late PE, although no previous studies have associated CRT with PEs. However, if patients require LVAD implantation despite undergoing CRT, their burden of comorbidities may be higher, which may influence the occurrence of late PE. Hypoalbuminemia, which results in decreased plasma osmotic pressure, was another predictor of late PE, consistent with previous findings [23,24]. The 90-day survival rate did not differ significantly between patients with and without late PE. Compared to patients without late PE, the rate of reintubation within 14 days was significantly higher (31.8% vs. 4.1%, P=0.004) and hospital, ICU, and ward stays were significantly longer in patients with late PE. Among the predictors of late PE, only albumin level is modifiable, suggesting that preoperative albumin correction might reduce the length of hospital stay.
This study had several limitations. The study was conducted at a single center and had a small sample size, which may limit the generalizability of the findings. Further large-scale studies are needed to validate the clinical outcomes observed here. Furthermore, we included patients who underwent heart transplantation, which could have influenced clinical outcomes. However, there was no significant difference in the rate of heart transplantation or the duration of surgery between the TD and no TD groups, suggesting a minimal impact on clinical outcomes.
More than half of the patients undergoing LVAD implantation needed TD. Patients who required TD had a longer hospital stay. No significant association with 90-day mortality was observed in patients undergoing TD. Early PEs were mostly characterized as exudate- and neutrophil-dominant, while lymphocyte-dominant composition was the most common finding in late PE. Correction of preoperative albumin level may contribute to a shorter hospital stay. Future studies with larger sample sizes and investigations of newer LVAD devices, such as HM3, are warranted to analyze the risk factors associated with poor prognosis.
KEY MESSAGES
▪ Despite the increasing use of left ventricular assist devices (LVADs) as a treatment option for advanced heart failure, research on LVAD-related pleural effusion (PE) is limited.
▪ Patients with therapeutic drainage (TD) experienced a prolonged hospital stay, but there was no difference in 90-day mortality between the TD and no TD groups.
▪ Patients with late PE had a higher rate of reintubation within 14 days and a longer hospital stay, with specific characteristics depending on the stage of effusion.
▪ Female sex, low body mass index, cardiac resynchronization therapy, and hypoalbuminemia were associated with late PE.
Notes
CONFLICT OF INTEREST
Min-Seok Kim is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflict of interest relevant to this article was reported.
FUNDING
This work was supported by the Asan Institute for Life Sciences, Asan Medical Center, Seoul, Korea (2018OM0234).
AUTHOR CONTRIBUTIONS
Conceptualization: SML, ARK, MSK. Methodology: SML, ARK, JH, MSK. Formal analysis: SML, ARK, JH, MSK. Data curation: SML, ARK, MSK. Visualization: SML, ARK, MSK. Project administration: SML, ARK, MSK. Funding acquisition: SML, ARK, MSK. Writing–original draft: all authors. Writing–review & editing: all authors.
Acknowledgements
None.