Effect of Timing of Do-Not-Resuscitate Orders on the Clinical Outcome of Critically Ill Patients
Article information
Abstract
Background:
Many physicians hesitate to discuss do-not-resuscitate (DNR) orders with patients or family members in critical situations. In the intensive care unit (ICU), delayed DNR decisions could cause unintentional cardiopulmonary resuscitation, patient distress, and substantial cost. We investigated whether the timing of DNR designation affects patient outcome in the medical ICU.
Methods:
We enrolled retrospective patients with written DNR orders in a medical ICU (13 bed) from June 1, 2014 to May 31, 2015. The patients were divided into two groups: early DNR patients for whom DNR orders were implemented within 48 h of ICU admission, and late DNR patients for whom DNR orders were implemented more than 48 h after ICU admission.
Results:
Herein, 354 patients were admitted to the medical ICU and among them, 80 (22.6%) patients had requested DNR orders. Of these patients, 37 (46.3%) had designated DNR orders within 48 hours of ICU admission and 43 (53.7%) patients had designated DNR orders more than 48 hours after ICU admission. Compared with early DNR patients, late DNR patients tended to withhold or withdraw life-sustaining management (18.9% vs. 37.2%, p = 0.072). DNR consent forms were signed by family members instead of the patients. Septic shock was the most common cause of medical ICU admission in both the early and late DNR patients (54.1% vs. 37.2%, p = 0.131). There was no difference in in-hospital mortality (83.8% vs. 81.4%, p = 0.779). Late DNR patients had longer ICU stays than early DNR patients (7.4 ± 8.1 vs. 19.7 ± 19.2, p < 0.001).
Conclusions:
Clinical outcomes are not influenced by the time of DNR designation in the medical ICU. The late DNR group is associated with a longer length of ICU stay and a tendency of withholding or withdrawing life-sustaining treatment. However, further studies are needed to clarify the guideline for end-of-life care in critically ill patients.
Introduction
As critical care medicine advances, concerns about the ethics of resuscitating terminally ill patients has also increased. [1] When death is imminent, cardiopulmonary resuscitation or critical care interventions to maintain a patient’s organ function can be regarded as futile by physicians or family members. However, end-of-life (EOL) care practices are complex and are influenced by multiple factors, including the physicians’ personal attitudes, family decisions, economic status, hospital policy, societal culture, and legislation.[2,3] For these reasons, the decision for do-not-resuscitate (DNR) orders and the withholding or withdrawal of life-sustaining management remains both a challenge and an important issue in intensive care units (ICUs).
It has been demonstrated that futile care in the ICU is associated with delays in appropriate management of other patients requiring critical care[4] and is related to substantial costs in the health care system.[5] Futile critical care also causes moral distress among nurses and could cause an ethical conflict between the ICU physicians and patient families.[6] Although EOL decisions in the ICU are important, a number of physicians hesitate to talk with families about DNR orders when the patient’s condition is acutely deteriorating. Specifically, ICU physicians in Asia tend to allow life-sustaining treatments at the EOL more frequently than physicians in Western countries.[2,7,8] Many Asian physicians also decide to withhold life-sustaining treatments rather than withdraw therapy.[2,7]
There have been a few articles about the relationship between the time of DNR designation and mortalities. [9,10] Accordingly, we investigated whether the timing of DNR orders affects the clinical outcomes of the patients in the medical ICU.
Materials and Methods
1) Study design and population
We performed a retrospective review of the medical records of patients who were admitted to a medical ICU with DNR orders from June 1, 2014 to May 31, 2015. The study was conducted in the medical ICU (13-bed, adult patients) of an academic tertiary referral hospital in Korea. When the patients were admitted to the ICU for any reason, the data of the patients’ implemented DNR orders were extracted. Patients who died within 24 hours of ICU admission were excluded.
This study was approved by the Institutional Review Board of Asan Medical Center (IRB NO: 2016-0027). Informed consent was waived due to the retrospective nature of the study.
2) Data collection
The following data for the patients admitted to the medical ICU were retrieved from the electronic medical records: age, sex, time of DNR order, Acute Physiology and Chronic Health Evaluation (APACHE II) score, route of ICU admission (via an emergency department or general ward), number of ICU readmissions, hospital length of stay before ICU admission, degree of limits on care (DNR and withdrawal or withholding of life-sustaining treatment), relation of family that signed the DNR form (patient, spouse, son/daughter, brother/sister, parents), major causes of ICU admissions, comorbidity; and ICU management, including hemodialysis, extracorporeal membrane oxygenation, mechanical ventilation, tracheostomy, vasopressors, inotropes, transfusion, analgesics, sedatives, central line insertion, and arterial line insertion.
The primary outcome was in-hospital mortality at the time of discharge. Three-month mortality and six-month mortality were also investigated. Hospital stay and ICU stay were measured as secondary outcomes.
The APACHE II score was based on the worst value obtained during the first 24 hours after ICU admission. If a patient had more than one ICU admission episode, only the episode associated with DNR orders and outcomes was considered.
3) Statistical analysis
Statistical analysis was performed using IBM SPSS statistics for Windows, version 21.0 (IBM, Armonk, NY, USA). A p-value less than 0.05 was considered statistically significant. Continuous variables were expressed as the mean ± standard deviation and categorical variables were expressed as the number (%). Patients were divided into an early DNR group and a late DNR group on the basis of 48 hours of ICU admission. The Student’s t-test for continuous variables and chi-square test for categorical variables were performed to compare differences of characteristics and outcomes between the two groups.
Results
Among a total of 354 patients admitted to a medical ICU, 80 (22.6%) patients with written DNR orders were enrolled. Two patients were excluded because they died within 24 hours. Finally, thirty-seven (46.3%) patients had DNR orders written within 48 hours of ICU admission, and 43 (53.7%) patients had DNR orders written more than 48 hours after ICU admission (Fig. 1).
Flowchart of enrolled patients in this study. early DNR orders: implemented within 48 h of ICU admission; late DNR orders: implemented more than 48 h after ICU admission; ICU: intensive care unit; DNR: do-notresuscitate.
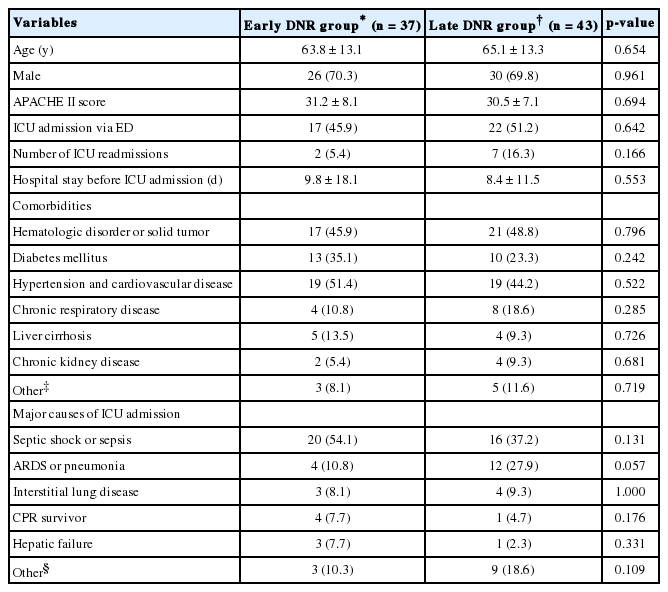
Comparison of baseline characteristics of the patients with DNR orders in the medical ICU are summarized in Table 1. There were no significant differences between two groups with regard to age, gender, and comorbidities. At the time of ICU admission, there was no difference in APACHE II scores between the two groups (31.2 ± 8.1 vs. 30.5 ± 7.1, p = 0.694). Septic shock was the most common cause of medical ICU admission in both groups (54.1% vs. 37.2%, p = 0.131). All DNR consents were signed by family members instead of the patients, most often by their sons and daughters. Large numbers of patients had hypertension and diabetes mellitus, and more than 40% of patients had solid tumors or hematologic malignancy.
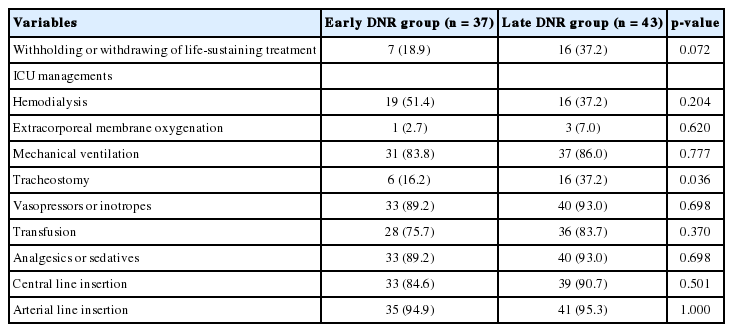
Compared with early DNR patients, late DNR patients tended to withhold or withdraw life-sustaining management (18.9% vs. 37.2%, p = 0.072). Management in the ICU was not different between the groups, except for tracheostomy (16.2% vs. 37.2%, p = 0.036) (Table 2).
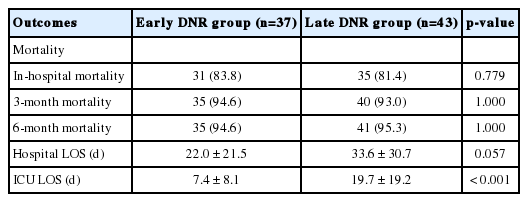
There were no differences in in-hospital mortality (83.8% vs. 81.4%, p = 0.779), 3-month mortality (94.6% vs. 93.0%, p = 1.000), and 6-month mortality (94.6% vs. 95.3%, p = 1.000) between the two groups. The late DNR group stayed longer in the medical ICU than the early DNR patients (7.4 ± 8.1 vs. 19.7 ± 19.2, p < 0.001) (Table 3).
Discussion
In this study, we identified that there was no difference in mortality between the early and late DNR groups. On the other hand, the late DNR group had a higher rate of tracheostomy and a tendency of withholding or withdrawing life-sustaining treatment. It has been demonstrated that DNR orders written later during hospitalization are different from those written shortly after admission.[9,11] The former is associated with a failure of full intensive care and a transition away from aggressive care, but the latter may be associated with a limit of critical care based on the pre-existing illness.[9,11]
Previously, a study showed that DNR orders written within 24 hours in septic shock patients are associated more strongly with increased in-hospital mortality than in patients without early DNR orders (65.3% vs. 37.5%).[10] Another study showed that pneumonia patients with written DNR orders after 24 hours of hospitalization had higher in-hospital and 90-day mortalities than early DNR groups.[9] In our study, we divided enrolled patients into an early DNR group and a late DNR group based on 48 hours of ICU admission. Because patients who died in less than 24 hours were at high risk of death at admission, we excluded these patients regardless of DNR order. Sufficient time for the decision to forgo life-sustaining treatment should be given to the patients and families, so we used 48 hours as the cutoff.[12]
As shown in our results, a major cause of medical ICU admission was septic shock, which requires full intensive care, especially in the initial phase. If a patient with septic shock no longer responds to initial resuscitation, poor outcomes are expected as a result of multiple organ system failure or severe neurologic injuries. Hence, the Surviving Sepsis Campaign emphasized the early recognition and early resuscitation. They also recommend that goals of care and prognosis should be discussed with patients and families.[13] Therefore, we emphasize that timely discussion of treatment goals, including DNR decisions and advance directives after ICU admission, is necessary to promote communication and understanding between the ICU physicians and the patients’ families.[13-15]
According to a recent report, 20% of ICU patients received futile or probably futile treatments, and as a result, delays in ICU admission from the emergency department or transfer from outside hospitals occurred.[4] The cost of futile critical care is also substantial. Hyunh et al.[5] reported that the cost of one day of treatment in the ICU that was perceived to be futile was more than $4,000. During the study period, total costs of futile critical care were 3.5% of total hospital costs. It is presumed that these are the major reasons for the high frequency of withholding or withdrawing life support in the late DNR group. The critical care is societal and with limited resources. Hence, the delivery of futile care may be harmful to other patients and may be a waste of societal resources.[16] Therefore, ICU physicians should be aware of which patients will benefit from high-intensity critical care.
In fact, EOL care practices (including DNR, withholding or withdrawing of life-sustaining treatments and advance directives) in the ICU are difficult to decide for a physician or family alone. There are several factors that influence EOL decision-making, e.g., age, comorbidity, functional status, socioeconomic status, religion, legislation, and degree of family’s involvement.[2] Compared to Western countries, ICU physicians in many Asian countries tend to be more aggressive with treatment. Results of the present study correspond with a previous study that suggested 20% of the late DNR group had implemented DNR orders on the eve of death. The reasons are that a number of ICU physicians were uncomfortable talking about EOL and legal risks in Asian countries.[2]
Four principles in ethical decision making are respect for autonomy (the patients’ right to self-determination), beneficence (the physicians’ duty to help patients whenever possible), non-maleficence (the obligation to avoid harm), and distributive justice (the fair allocation of medical resources).[17] In our data, an important finding is that all DNR consents were written by family members instead of the patients. A large number of critically ill patients are not able to make decisions for themselves because of their illness or sedated states.[18] Hence, the families make decisions as surrogates for ICU patients who cannot participate in EOL discussions.[12] They want to protect the patients from knowing their life-limiting illness[19] and may prolong dying even if opposed to the patient’s own volition. Also, the traditional Asian values of filial piety and responsibility toward patients may contribute to this condition.[20] A reason for disregarding autonomy in this study was probably due to the culture of advance directives that was not widely settled yet in Korea.
In our data, approximately 30% of the medical ICU patients with DNR orders had advanced malignancies. However, advance directives were not discussed before ICU admission, even in patients with malignancies in terminal stages. Blackhall et al.[21] investigated that Korean Americans were less likely to inform elderly patients of the diagnosis or prognosis of terminal illness than European or African Americans. Compared to the United States, there were lower rates of advance directives completed in Asia.[20] Critically ill patients should be informed of their underlying diagnosis and prognosis before ICU admission. They should prepare their EOL and decide on the limitations of life-sustaining treatments with ICU physicians and their families.
This study has several limitations, mostly stemming from its retrospective design. Because there were no specific guidelines for EOL practices in critically ill patients, most DNR orders or limitations of life-sustaining treatment were initiated by the ICU physicians’ decision. Although the APACHE II score was not significantly different between two groups, more severe patients might be enrolled in the early DNR group. Furthermore, EOL practices could be altered based on the physician’s region of practice, religion, or families’ desire.[22,23] Second, because patients admitted to the medical ICU were enrolled, this study does not reflect results of surgical ICU patients. Third, this study was conducted in a single-center, tertiary referral hospital, and severity of illness or practices may be different from other centers’ data. Therefore, a prospective cohort study involving all types of ICUs in multiple centers is necessary.
In conclusion, clinical outcomes are not influenced by the time of DNR designation in the medical ICU. The late DNR group is associated with a longer length of ICU stay and a tendency of withholding or withdrawing life-sustaining treatment. However, further studies are needed to clarify the guideline for end-of-life care in critically ill patients.
Notes
No potential conflict of interest relevant to this article was reported.